If you buy through links on our site, we may earn a small affiliate commission to help support the blog - at no extra cost to you. It never influences our product selection process. Thank you!
Discovering a hole in your tooth can be alarming, especially when accompanied by pain or sensitivity. This common dental issue, known as a cavity or dental caries, affects millions of Americans each year and shouldn’t be ignored.
When tooth enamel breaks down due to acids produced by bacteria, these tiny holes can form and gradually worsen without proper treatment. While poor oral hygiene is often the primary culprit, factors like sugary diets, dry mouth, and genetics can also contribute to this problem. Understanding why these holes develop is the first step toward protecting your smile and preventing further damage.
Understanding Tooth Cavities: Why Holes Form
Tooth cavities form when bacteria in your mouth produce acids that gradually dissolve tooth enamel, creating small holes that can grow larger over time. These acids attack the tooth’s protective outer layer, penetrating deeper into the dentin and potentially reaching the sensitive pulp inside. Many patients notice these holes while brushing or flossing, often accompanied by sensitivity to hot, cold, or sweet foods.
Dr. Todd B. Harris often tells patients, “Cavities don’t develop overnight—they’re the result of an ongoing process that can be intercepted with proper care.” One patient, Sarah, discovered a small hole in her molar during a routine self-examination and wisely scheduled an immediate appointment, preventing what could have become a serious infection requiring root canal therapy.
The Cavity Formation Process
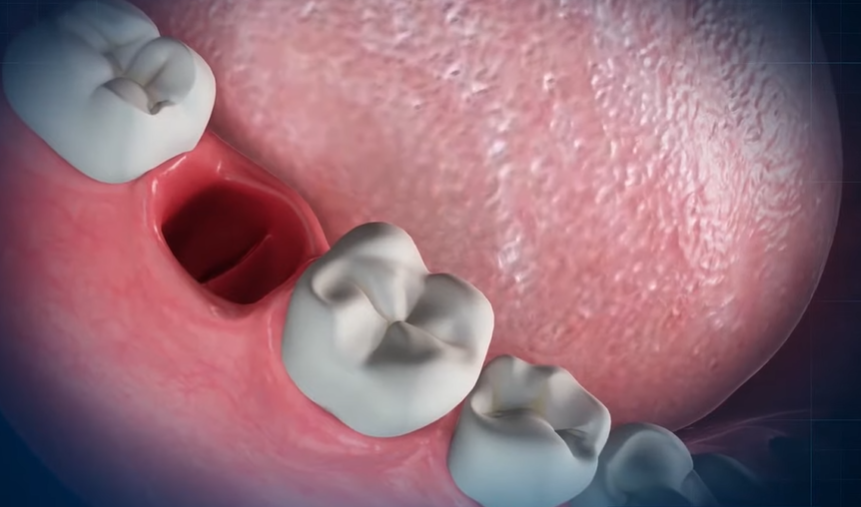
Cavity formation begins with plaque accumulation on tooth surfaces. This sticky bacterial film produces acids when exposed to sugars and carbohydrates in your diet. Constant acid attacks gradually demineralize enamel, creating microscopic openings that eventually become visible holes. Left untreated, these holes expand and deepen, compromising tooth structure and function.
Dental professionals classify cavities into three main types:
- Pit and fissure cavities occur on chewing surfaces
- Smooth surface cavities develop on the flat sides of teeth
- Root cavities form below the gumline on exposed tooth roots
Risk Factors for Cavity Development
Several factors increase your likelihood of developing tooth cavities:
| Risk Factor | Impact Level | Prevention Strategy |
|---|---|---|
| Poor oral hygiene | Very High | Brush twice daily, floss once daily |
| High-sugar diet | High | Limit sugary foods and drinks |
| Dry mouth | Moderate | Stay hydrated, use saliva substitutes |
| Lack of fluoride | Moderate | Use fluoride toothpaste, get professional treatments |
| Frequent snacking | Moderate | Reduce between-meal eating |
| Worn dental work | Moderate | Replace old fillings and crowns |
Genetics also plays a role in cavity susceptibility. Some people naturally have weaker enamel or deeper tooth grooves that trap food particles more easily. Also, certain medications can reduce saliva production, diminishing your mouth’s natural ability to neutralize acids and remineralize enamel.
Common Causes of Holes in Teeth

Holes in teeth are primarily caused by dental cavities, which are areas where tooth decay has damaged the hard surface of your enamel. These tiny openings develop gradually and can lead to important dental problems if left untreated. Let’s examine the main factors contributing to these troublesome dental holes.
Tooth Decay and Dental Caries
Dental caries form when acids produced by bacteria in plaque break down your tooth enamel. This process begins with plaque, a sticky film that adheres to teeth and harbors bacteria. The bacteria feed on sugars and starches from your diet, producing acids that attack and weaken the enamel. Over time, these acid attacks create small holes in your teeth that can expand deeper into the tooth structure. Many patients don’t notice these early stages of decay until the cavity has progressed significantly, which is why regular dental check-ups are crucial for early detection.
Poor Oral Hygiene Habits
Inadequate brushing and flossing allows plaque to build up on your teeth, significantly increasing your risk of developing cavities. When you skip brushing or don’t clean all surfaces of your teeth properly, bacteria thrive in these neglected areas. Plaque can harden into tartar within 24-72 hours, creating a shield for bacteria that’s impossible to remove with regular brushing. Dr. Todd B. Harris often notes that many patients with cavities admit to inconsistent oral hygiene routines, especially skipping nighttime brushing when cavity-causing bacteria are most active during sleep.
Diet and Sugar Consumption
Your eating habits play a crucial role in cavity formation. Frequent consumption of sugary foods and drinks provides fuel for bacteria to produce more acid, accelerating enamel erosion. Carbohydrate-rich foods like bread, chips, and crackers also break down into simple sugars that feed harmful bacteria. Constantly sipping on acidic or sugary beverages throughout the day is particularly damaging as it creates a continuous acid environment in your mouth. One patient shared how switching from drinking soda all day to limiting it to mealtimes significantly reduced their cavity formation after years of dealing with recurring dental holes.
Recognizing the Signs of a Cavity

Identifying a cavity early can save you from extensive dental procedures and pain. Cavities develop gradually, often with subtle signs that become more noticeable as decay progresses.
Visual Changes in Your Tooth
Visual indicators of a cavity are typically the first warning signs you’ll notice. Visible holes or pits in your tooth surface indicate that decay has already damaged the enamel structure. Discoloration appears as brown, black, or white stains on the affected tooth, signaling areas where minerals have been lost due to acid attack. Small dark spots on tooth surfaces often indicate the beginning stages of decay, even before a hole forms completely. Transparent or chalky white areas on teeth suggest demineralization is occurring, an early stage of cavity formation.
One of my patients, Sarah, noticed a small black dot on her molar while flossing but ignored it for months, assuming it was just a stain. By the time she came in for her check-up, that tiny spot had developed into a important cavity requiring a large filling.
Pain and Sensitivity Symptoms
Pain and sensitivity develop as cavity damage extends deeper into tooth layers. Tooth sensitivity occurs when consuming hot, cold, or sweet foods and beverages, indicating that enamel has thinned enough to affect the dentin layer beneath. Sharp pain when biting down suggests decay has reached deeper tooth layers where nerves are located. Persistent toothaches, even without stimuli, often mean infection has developed in the tooth’s pulp. Lingering pain after consuming triggering foods typically indicates advanced decay that may require root canal treatment.
Temperature sensitivity serves as a reliable early warning system for many patients. Dental pain rarely resolves on its own and typically worsens over time as the cavity enlarges. Morning tooth discomfort frequently indicates nighttime grinding that can accelerate cavity formation in already weakened teeth.
The Progression of Tooth Decay

Tooth decay follows a predictable pattern, transforming from minor enamel damage to potentially serious dental issues. Understanding this progression helps you recognize problems early and take appropriate action before extensive damage occurs.
From Enamel Damage to Deep Cavities
Initial demineralization marks the beginning of tooth decay, appearing as white spots where acids from bacteria have started dissolving minerals in your enamel. These spots indicate the earliest stage of damage, which can sometimes be reversed through fluoride treatments and improved oral hygiene.
Continued acid exposure leads to enamel decay, turning those white spots brown as small holes (cavities) begin to form. Once these cavities develop, they can’t naturally reverse and require dental fillings to restore your tooth structure.
When decay advances beyond the enamel, it reaches the dentin layer underneath. This progression often triggers sensitivity and pain because dentin contains many nerve endings that respond to temperature changes and sweet foods.
Deeper decay affects the pulp—the innermost part of your tooth containing nerves and blood vessels. Pulp damage typically causes severe pain and often necessitates root canal treatment or extraction to save the affected tooth.
Left untreated, decay eventually leads to infection and abscess formation. Dental abscesses present with swelling, intense pain, and sometimes fever, requiring emergency dental care to prevent the infection from spreading.
How Fast Can a Hole Develop?
Cavity development varies significantly among individuals, influenced by factors like oral hygiene practices, dietary habits, fluoride exposure, and genetic susceptibility. Early stages of demineralization typically take weeks to months to become visible.
Once your enamel begins breaking down, holes can develop more rapidly, sometimes forming within months if plaque buildup and acid exposure continue without intervention. Dr. Todd B. Harris often tells patients, “I’ve seen young patients develop important cavities in just 4-6 months after abandoning their oral hygiene routines during stressful academic periods.”
Frequent consumption of acidic beverages accelerates this timeline dramatically. A patient once shared, “I was shocked when my dentist found three cavities after I spent a summer drinking lemonade and sports drinks constantly—my teeth had been perfectly healthy at my check-up just six months earlier.”
The progression accelerates once decay penetrates the enamel, as dentin is softer and more vulnerable to acid damage. Regular dental check-ups every six months prove crucial for catching decay in its earliest stages, when treatment options are less invasive and more affordable.
Treatment Options for Tooth Holes

Treating a hole in your tooth promptly prevents further decay and relieves discomfort. Several effective treatment options exist depending on the severity of the cavity and how far the decay has progressed.
Dental Fillings and Restorations
Dental fillings are the most common treatment for cavities and tooth holes. Your dentist removes the decayed portion of the tooth and fills the space with durable materials to restore functionality and appearance. Composite resin fillings match your natural tooth color, making them virtually invisible in your smile. Silver amalgam fillings offer exceptional durability, particularly for back teeth that endure important chewing forces. Gold fillings, though more expensive, provide longevity with some patients reporting their gold fillings lasting 20+ years. The filling procedure typically takes just one appointment, with the dentist first numbing the area, removing decay, cleaning the cavity, and then placing the chosen filling material.
Root Canal Therapy for Advanced Cases
Root canal therapy becomes necessary when decay penetrates through the enamel and dentin layers to reach the tooth’s pulp. This treatment saves teeth that would otherwise require extraction by removing infected pulp tissue and sealing the canal. During the procedure, your dentist creates a small access hole, removes the infected pulp, cleans the canal system, and fills it with a biocompatible material called gutta-percha. Most teeth that undergo root canal treatment require a crown afterward to provide structural support and prevent fractures. Modern root canal procedures use advanced anesthetics and techniques, making them no more uncomfortable than receiving a standard filling. Approximately 25 million root canal procedures are performed annually in the United States, with a success rate exceeding 95% when performed by experienced dental professionals.
Preventing Holes in Your Teeth

Preventing tooth holes from cavities requires consistent oral hygiene practices and professional dental care. Proactive prevention strategies protect your enamel from decay-causing bacteria and acids that lead to cavities.
Effective Brushing and Flossing Techniques
Brushing your teeth twice daily with fluoride toothpaste strengthens your enamel and removes harmful plaque buildup. Fluoride works directly to reinforce tooth structure, making it more resistant to acid attacks from bacteria. Using proper brushing technique—gentle circular motions for at least two minutes—ensures you’re cleaning all tooth surfaces effectively.
Daily flossing removes plaque from between teeth where your toothbrush can’t reach. These tight spaces between teeth often become breeding grounds for bacteria that cause decay when left undisturbed. Proper flossing involves gently sliding the floss between teeth and curving it around each tooth in a C-shape to remove hidden food particles and bacteria.
Dr. Harris often shares that “many patients with recurring cavities are surprised to learn they’ve been brushing incorrectly for years. One patient dramatically reduced their cavity rate simply by adding proper flossing to their routine after skipping it for decades.”
Regular Dental Check-ups
Visiting your dentist every six months allows for professional cleaning and early detection of potential problems. Professional dental cleanings remove hardened tartar (calcified plaque) that regular brushing and flossing can’t eliminate on their own.
Dental professionals spot early signs of decay during routine exams, often before you notice any symptoms. X-rays help dentists identify cavities forming between teeth or beneath existing fillings where they remain invisible to the naked eye. Early intervention with treatments like fluoride applications can sometimes reverse initial enamel demineralization before a cavity fully forms.
“I’ve seen countless teeth saved because we caught decay during a routine check-up,” notes Dr. Harris. “One patient came in for their regular cleaning feeling perfectly fine, but we discovered three developing cavities that would have eventually caused important pain and required extensive treatment if left unaddressed.”
Limiting frequent snacking, especially on sticky sugary foods, creates fewer opportunities for acid production in your mouth. Drinking water after meals helps wash away food particles and neutralize acids. Choosing sugar-free gum containing xylitol can stimulate saliva flow, which naturally protects your teeth by neutralizing acids and remineralizing enamel.
When to See a Dentist About a Tooth Hole
Dental pain or discomfort from a tooth hole shouldn’t be ignored, as early intervention prevents more serious complications. You’ll need to schedule a dental appointment immediately if you experience persistent toothache, especially when eating or biting down on food. Sensitivity to hot, cold, sweet, or sour foods and drinks often indicates decay has progressed beyond the enamel layer and requires professional attention.
Visible holes, pits, or discoloration (appearing as brown, black, or white stains) on your teeth are clear signs that decay has begun and dental evaluation is necessary. Bad breath or an unpleasant taste in your mouth might result from food particles and bacteria trapped in cavities, signaling it’s time to see your dentist. Facial swelling, pus, or signs of infection represent advanced complications that demand emergency dental care.
Dr. Todd B. Harris notes, “Many patients come in only after experiencing important pain, but I recently treated a patient who noticed a small dark spot during routine brushing. By addressing this early cavity promptly, we avoided extensive treatment and saved the integrity of her tooth. This reinforces why I recommend regular checkups even when no symptoms are present.”
Regular dental checkups remain crucial since cavities often form without noticeable symptoms initially. Your dentist can detect early signs of decay through visual examination and dental X-rays before holes become visible to the naked eye. Postponing treatment for a tooth hole typically leads to worsening decay, which may eventually require more extensive and expensive procedures like root canals or extractions.
Conclusion
A hole in your tooth signals that decay has compromised your dental health. Don’t ignore this warning sign. Addressing cavities promptly with proper treatment prevents further damage and preserves your natural tooth structure.
Remember that prevention remains your best defense against tooth decay. Maintain diligent oral hygiene habits brush twice daily use fluoride toothpaste and floss regularly. Limit sugary foods drink plenty of water and don’t skip those twice-yearly dental checkups.
Your smile deserves protection. By understanding what causes cavities and taking proactive steps you’ll maintain stronger healthier teeth for years to come. If you suspect you have a cavity don’t wait—schedule a dental appointment today.
Frequently Asked Questions
What causes cavities in teeth?
Cavities form when bacteria in your mouth produce acids that break down tooth enamel. This process begins with plaque accumulation, which creates acids when exposed to sugars and carbohydrates. Poor oral hygiene is the primary cause, but factors like sugary diets, dry mouth, frequent snacking, and genetics also contribute. Without proper care, these small holes can grow larger over time and compromise tooth structure.
How can I identify if I have a cavity?
Look for visual signs like holes, pits, or discoloration on tooth surfaces. Early cavities may cause sensitivity to hot, cold, or sweet foods and beverages. As decay progresses, you might experience sharp pain when biting down or persistent toothaches. White spots on teeth can indicate early demineralization. If you notice any of these symptoms, schedule a dental appointment for proper diagnosis.
What are the different types of cavities?
Dentists classify cavities into three main types: 1) Pit and fissure cavities that develop on chewing surfaces, 2) Smooth surface cavities that form on the flat sides of teeth, and 3) Root cavities that occur below the gumline on exposed root surfaces. Each type requires specific treatment approaches, but all result from the same decay process caused by bacterial acids eroding tooth structure.
How does tooth decay progress if left untreated?
Tooth decay follows a predictable progression. It begins with demineralization (white spots) that can sometimes be reversed with fluoride. If untreated, enamel breaks down, forming a cavity requiring a filling. As decay advances to the dentin layer, sensitivity increases. When decay reaches the pulp, severe pain develops, often necessitating root canal therapy or extraction. The progression rate varies among individuals.
What treatments are available for cavities?
For early to moderate cavities, dental fillings are the standard treatment. The dentist removes decayed material and fills the space with composite resin or amalgam. More extensive decay may require a crown to restore tooth structure. When decay reaches the pulp, root canal therapy becomes necessary to remove infected tissue and save the tooth. Severely damaged teeth that cannot be restored may require extraction.
How can I prevent cavities from forming?
Prevent cavities by brushing twice daily with fluoride toothpaste, flossing daily to remove plaque between teeth, and visiting your dentist every six months for check-ups and professional cleanings. Limit sugary foods and beverages, avoid frequent snacking, and drink water after meals to wash away food particles. Consider dental sealants for additional protection, especially for children’s molars with deep grooves.
When should I see a dentist about a potential cavity?
See a dentist immediately if you experience persistent tooth pain, sensitivity to temperature, visible holes or discoloration, or bad breath/unpleasant taste that doesn’t go away with brushing. Don’t wait until pain becomes severe—early intervention leads to simpler, less expensive treatments. As Dr. Todd B. Harris notes, “Regular check-ups can catch problems before they require extensive treatment.”
Can cavities heal on their own?
Very early stages of tooth decay (demineralization) can sometimes be reversed with proper oral hygiene and fluoride treatments. However, once a true cavity forms—creating a hole in the enamel—it cannot heal naturally and requires professional dental treatment. The tooth structure does not regenerate, which is why prevention and early intervention are crucial for maintaining dental health.