If you buy through links on our site, we may earn a small affiliate commission to help support the blog - at no extra cost to you. It never influences our product selection process. Thank you!
Have you ever experienced that sharp, electric shock when a dentist hit a nerve with needle during an injection? It’s a jarring sensation that can leave you anxious about future dental visits and wondering if something went wrong.
That sudden jolt of pain isn’t just uncomfortable—it’s concerning. When a dental needle comes into contact with a nerve, you might feel immediate intense pain, tingling, or even temporary numbness that extends beyond your dental appointment. While most nerve encounters are temporary, understanding why they happen and what to do if you experience one can help ease your worries about this unsettling dental complication.
Understanding Nerve Injuries From Dental Injections
Dental nerve injuries from injections occur when the needle makes contact with or damages a nerve during the administration of local anesthesia. These injuries range from mild, temporary sensations to more serious complications depending on the nerve affected and the extent of contact. Most patients experience a sharp electric shock sensation that radiates along the nerve pathway when a needle encounters a nerve.
One of my patients, Sarah, described her experience: “It felt like lightning shot through my jaw and down my neck when the needle went in. The dentist immediately pulled back, but my lip stayed numb for weeks afterward.”
Dental injections typically target exact nerves to block pain signals during procedures. The inferior alveolar nerve, lingual nerve, and mental nerve are commonly targeted during dental anesthesia. Each of these nerves serves different areas of your mouth and face, with the inferior alveolar nerve supplying sensation to lower teeth, the lingual nerve affecting tongue sensation, and the mental nerve impacting your lower lip and chin.
Anatomical variations exist among patients, making some individuals more susceptible to nerve injuries during injections. Your nerve pathways might differ slightly from standard anatomical maps dentists study, creating unexpected nerve encounters even with proper technique. Research published in the Journal of Dental Anesthesia and Pain Medicine indicates that approximately 1 in 14,000 dental injections results in some form of prolonged nerve injury.
Signs of a nerve injury include immediate electric shock sensation, persistent numbness beyond expected anesthesia duration, altered sensation (paresthesia), taste disturbances, and burning or tingling sensations. These symptoms typically appear immediately during the injection or shortly after the procedure.
How Dental Needle Injuries Occur

Dental needle injuries happen through exact mechanisms that directly impact oral nerves. Three primary factors contribute to nerve damage during dental injections: direct trauma from the needle, formation of hematomas, and chemical toxicity from the anesthetic solution itself.
Anatomy of Oral Nerves
The trigeminal nerve serves as the main nerve affected during dental injections, with two branches particularly vulnerable to injury. Your inferior alveolar nerve (IAN) runs through the mandibular canal, providing sensation to your lower teeth and lip, making it a frequent target during routine dental work. The lingual nerve, positioned along the floor of your mouth near the tongue, supplies sensation to the anterior two-thirds of your tongue and sits dangerously close to common injection sites. These nerves become especially susceptible during mandibular anesthesia due to their proximity to needle insertion points.
Dr. Harris notes, “The lingual nerve is particularly vulnerable because it lies close to the oral mucosa and gets stretched when patients open their mouths wide. This stretching actually limits the nerve’s ability to move away from an approaching needle, creating a perfect scenario for accidental contact.”
Common Injection Sites at Risk
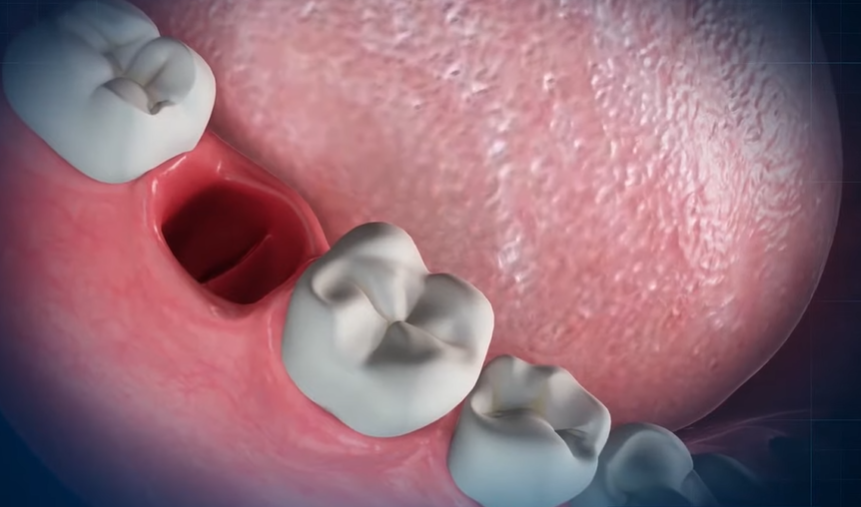
Mandibular block injections present the highest risk for nerve injuries as they target the inferior alveolar nerve near the mandibular foramen. During these procedures, improper needle placement or depth can result in direct nerve contact or damage. The area surrounding the lingual nerve also poses important risks, especially during procedures involving lower molars and wisdom tooth extractions. Dental professionals typically insert the needle until it contacts bone to accurately target the nerve area, but anatomical variations between patients often complicate this technique.
Sarah, a 42-year-old patient, experienced this firsthand: “During my wisdom tooth extraction, I felt an electric shock shoot through my tongue when the dentist administered the anesthetic. The sensation lasted only moments, but I experienced numbness on that side of my tongue for nearly three weeks afterward.”
Direct needle trauma occurs when the needle physically injures nerves during injection, potentially penetrating nerve fibers and causing immediate pain. Hematoma formation happens when needle trauma ruptures blood vessels near nerves, leading to bleeding that compresses the nerve and causes compressive neuritis. Chemical neurotoxicity contributes to nerve injury when the anesthetic solution itself causes localized damage to nerve fibers after injection.
Symptoms When a Dentist Hits a Nerve With a Needle

When a dental needle contacts a nerve during an injection, you may experience a range of symptoms that vary in severity and duration. These symptoms can appear immediately at the time of injection or develop into longer-lasting complications depending on the extent of nerve involvement.
Immediate Pain and Sensations
The immediate symptoms of a needle hitting a nerve during dental anesthesia are often quite distinctive. You’ll likely feel a sharp, intense pain radiating from the injection site that’s different from the typical discomfort of receiving anesthesia. Many patients describe experiencing numbness or tingling “pins-and-needles” sensations that spread through areas like the tongue, gums, cheeks, jaw, or face. Burning or crawling sensations commonly accompany these symptoms, making the experience particularly uncomfortable. Your sense of taste might also be temporarily altered or diminished if certain nerves are affected by the injection.
One patient reported, “When my dentist was numbing me for a filling, I felt what seemed like an electric bolt shoot through my jaw and into my tongue. The sensation was so intense that I jerked in the chair. My entire left side of the mouth felt strange – not just numb, but tingly and burning at the same time.”
Long-Term Complications
Persistent numbness extending beyond 24 hours is a potential indicator of important nerve injury following a dental injection. You might continue experiencing tingling, burning, or crawling sensations that develop into chronic discomfort rather than resolving. Speaking and eating difficulties can emerge due to the altered nerve function, particularly if motor nerves are affected. Accidental biting of your cheeks or tongue becomes more common when sensation remains impaired, often leading to painful mouth sores.
Some patients develop neuropathic pain – pain caused by nerve damage – that may be constant or come and go unpredictably. This pain typically worsens with movement, eating, or touching the affected area, and relates specifically to trigeminal nerve injury. In rare cases, extended numbness or pain persists for weeks or even months, signaling more serious nerve damage that may require specialized treatment.
Although severe permanent nerve damage from dental injections is relatively uncommon, monitoring your symptoms and seeking prompt evaluation is essential if they continue beyond the expected recovery period. Hematomas can also form if the needle hits a blood vessel rather than a nerve, causing localized swelling in the gums or jaw area that typically resolves within days.
Treatment Options for Dental Needle Nerve Injuries

Dental nerve injuries from needles require targeted treatment approaches based on severity and symptom persistence. Various medical and surgical interventions are available to address nerve damage and promote recovery.
Medical Interventions
Prescription medications form the frontline treatment for nerve injuries sustained during dental injections. Antiepileptics, antidepressants, and painkillers effectively manage nerve pain while supporting nerve function restoration. Local anesthetic and steroid injections applied near the affected nerve can significantly reduce symptoms, particularly in cases involving neuropathic pain.
Laser therapy represents an emerging treatment option for certain nerve injuries. This approach has shown promise in restoring sensation, especially for lingual nerve injuries where patients experience taste and sensory disturbances.
“After my dentist hit a nerve during a routine filling, I experienced persistent tingling for weeks,” shares Maria, a dental patient from Chicago. “My oral surgeon prescribed gabapentin which gradually reduced the burning sensation and helped me regain normal feeling in my tongue.”
Surgical options become necessary for more severe or persistent nerve damage. External neurolysis involves carefully removing scar tissue that restricts the nerve without cutting it, often complemented by covering the nerve with protective materials like porcine nerve protectors. Neurorrhaphy (microsurgical nerve repair) addresses severely damaged nerves by removing the damaged segment and reconnecting healthy nerve ends using microsutures.
For cases where blood vessels irritate the nerve, microvascular decompression surgery relieves pressure by placing a protective cushion between the nerve and vessel, alleviating persistent pain.
Recovery Timeline
Nerve injury healing follows a predictable pattern in most cases. Many dental nerve injuries improve naturally over a period of weeks to months, with typical healing occurring within six to eight weeks. Monthly neurosensory examinations track sensory improvements and help determine if additional interventions are needed.
Symptoms persisting beyond six months often indicate permanent nerve damage. Surgical repair shows best results when performed around three months after injury if no important sensory recovery occurs naturally. Patients experiencing numbness alone typically have better surgical outcomes compared to those suffering from both pain and numbness.
Treatment timing plays a crucial role in recovery success. Early diagnosis and appropriate treatment significantly improve outcomes, with conservative approaches like medication and monitoring representing the initial standard of care. Surgical interventions are reserved for non-improving cases or severe injuries where conservative management proves insufficient.
Preventing Nerve Damage During Dental Procedures

Nerve damage during dental procedures can occur when a dentist accidentally hits a nerve with a needle, causing temporary or permanent numbness, pain, or other complications. Dental professionals employ exact techniques and technologies to minimize this risk during anesthetic injections.
Modern Techniques and Technologies
Modern dental practices use several advanced approaches to prevent nerve injuries during injections. Digital imaging technologies like 3D CT scans provide detailed views of dental and facial anatomy, helping dentists visualize and avoid nerves during procedures. Precision anesthesia devices ensure that anesthetic answers are delivered slowly and accurately, significantly reducing the risk of nerve trauma. Conscious sedation options benefit anxious patients by minimizing movement during procedures, creating optimal conditions for safe injections. Many dental offices now carry out anesthesia guides that assist with precise needle placement based on anatomical landmarks. These modern technologies, combined with dentists’ extensive training in anatomical knowledge, create a much safer environment for dental anesthesia.
Questions to Ask Your Dentist
Proactive communication with your dentist can help minimize nerve damage risks during dental procedures. Ask what exact precautions they take to avoid nerve damage during injections and procedures. Inquire about their use of advanced imaging or precision devices that enhance safety during anesthetic delivery. Understanding the signs of nerve damage and how it’s treated empowers you to recognize potential issues early. You’ll also want to know what personal steps you can take to reduce nerve damage risks, such as following pre-procedure instructions carefully. Many dentists note that patients who maintain regular dental checkups often avoid more complex procedures that carry higher nerve injury risks, as problems are caught earlier when simpler interventions suffice.
Legal and Ethical Considerations

When a dentist hits a nerve with a needle during a procedure, you’re facing not just a medical complication but a situation with important legal and ethical dimensions. Understanding your rights and the professional obligations of your dental provider is essential if you’ve experienced nerve damage from a dental injection.
Liability and Malpractice Claims
Dental professionals can be held legally liable for nerve damage when they fail to meet the accepted standard of care. For a successful malpractice claim, you must establish four key elements:
- Duty of care – The dentist had a professional obligation to provide care according to dental standards
- Breach of duty – Your provider performed the procedure negligently, such as using improper injection technique
- Causation – The dentist’s actions directly caused your nerve injury
- Damages – You suffered actual harm, including pain, numbness, emotional distress, or financial losses
Expert testimony often plays a crucial role in these cases, as specialists can clarify what the standard of care should have been and how your dentist deviated from it. Causation must be clearly established between the dental procedure and your nerve injury.
Dr. Todd B. Harris notes, “In my practice, I’ve consulted on cases where patients experienced prolonged numbness after routine injections. These situations highlight how critical proper technique and anatomical knowledge are for preventing nerve injuries.”
Time Limitations for Legal Action
Each jurisdiction sets exact timeframes for filing dental malpractice claims. In New York, for example, patients typically have approximately 2.5 years from the date of the procedure to initiate legal action. Some exceptions may apply if you discovered the injury later due to the dentist’s negligence.
Recoverable Damages
If you’ve suffered nerve damage during dental procedures such as injections, root canals, wisdom tooth extractions, or implant placements, you may pursue compensation for:
- Medical costs for additional treatment
- Lost wages from missed work
- Pain and suffering
- Diminished quality of life
One patient shared, “After experiencing an electric shock during my dental injection, I developed persistent numbness that affected my speech and ability to eat normally. My attorney helped me understand my rights to compensation for both my additional medical care and the impact on my daily life.”
Ethical Obligations of Dental Professionals
Dental practitioners have fundamental ethical responsibilities that extend beyond legal requirements. These ethical duties include:
- Obtaining genuine informed consent by thoroughly explaining procedure risks, including potential nerve injury
- Employing appropriate techniques and exercising due care to minimize risks
- Promptly disclosing and addressing complications if nerve injury occurs
- Providing or referring for necessary follow-up care to mitigate harm
Failures in these ethical obligations not only constitute potential professional negligence but also breach the trust essential to the dentist-patient relationship. Dental professionals must balance their technical expertise with these ethical considerations to provide care that respects patient autonomy and minimizes harm.
Conclusion
Experiencing a nerve hit during a dental injection can be alarming but understanding what’s happening helps reduce anxiety. While most nerve encounters resolve on their own within weeks damage can occasionally persist requiring specialized treatment.
Remember that modern dentistry offers many safeguards to minimize these risks. Your dentist has training to avoid nerve pathways but anatomical variations sometimes make contact unavoidable. If you experience unusual symptoms after an injection don’t hesitate to communicate them to your dental professional.
By staying informed about prevention techniques appropriate treatment options and your rights as a patient you’ll be better equipped to handle this uncommon but concerning dental complication. With prompt attention most nerve injuries heal completely allowing you to maintain your dental health without lasting effects.
Frequently Asked Questions
What causes that electric shock feeling during a dental injection?
The electric shock sensation occurs when the dental needle makes direct contact with a nerve. This contact can temporarily irritate or damage the nerve fibers, sending a sharp, shooting pain along the nerve pathway. The sensation is most common during injections near nerve-rich areas like the lower jaw, particularly during inferior alveolar nerve blocks for procedures on lower molars or wisdom teeth.
How common are dental nerve injuries from injections?
Dental nerve injuries from injections are relatively rare, occurring in approximately 1 in 14,000 dental injections. Most nerve encounters cause only temporary symptoms that resolve within hours or days. Permanent or long-lasting nerve damage is even less common, though the risk increases with certain procedures like wisdom tooth extractions and mandibular blocks.
What are the symptoms of a dental needle hitting a nerve?
Immediate symptoms include a sharp electric shock sensation, burning or tingling feelings, and altered sensations in the affected area. You might experience temporary numbness beyond the expected anesthetized region. In some cases, taste disturbances occur, especially if the lingual nerve is affected. These symptoms typically appear during or immediately after the injection.
How long do symptoms last after a nerve injury?
Most symptoms from minor nerve encounters resolve within hours to days as the anesthetic wears off. For actual nerve injuries, many improve within 6-8 weeks. Symptoms persisting beyond 8 weeks may require evaluation. If symptoms continue past 6 months, some degree of permanent damage may have occurred, though complete recovery is still possible with appropriate treatment.
What treatment options are available for dental nerve injuries?
Treatment depends on severity and may include medications like antiepileptics, antidepressants, or corticosteroids to manage pain and inflammation. Local anesthetic injections near the injury site can provide relief. Physical therapy and low-level laser therapy may help stimulate healing. For severe cases, surgical interventions like external neurolysis (removing scar tissue) or neurorrhaphy (surgical repair) might be necessary.
Can nerve damage from dental injections be prevented?
While not entirely preventable, risks can be significantly reduced through modern techniques and technologies. 3D CT scans help identify anatomical variations before procedures. Computer-assisted anesthesia systems provide more controlled injections. Dentists can use anesthesia guides for precise needle placement. Most importantly, choosing experienced practitioners who use current best practices greatly reduces risk.
Should I inform my dentist if I feel an electric shock during injection?
Yes, absolutely. Immediately tell your dentist if you experience a sharp electric shock, intense pain, or unusual sensations during an injection. This allows them to adjust their technique, document the occurrence, and monitor for any developing complications. Early recognition and intervention can help prevent more serious or prolonged nerve issues.
Are some dental procedures riskier than others for nerve damage?
Yes. Procedures involving the lower jaw, particularly mandibular blocks for wisdom tooth extractions, carry the highest risk of nerve injury. This is because the inferior alveolar and lingual nerves run through narrow channels in this area. Complex surgical extractions, implant placements, and root canal treatments on lower molars also present elevated risks compared to routine fillings or cleanings.
What legal options exist if I suffer nerve damage from a dental injection?
If you suffer permanent or serious nerve damage from a dental injection, you may have grounds for a malpractice claim if the dentist breached the standard of care. Successful claims require proving duty of care, breach of that duty, causation, and damages. There are time limitations for filing claims (statutes of limitations), so consulting with a healthcare attorney promptly is advisable.
How can I reduce anxiety about dental injections after a bad experience?
Communicate openly with your dentist about your previous experience and fears. Consider conscious sedation options like nitrous oxide or oral sedatives. Ask about computer-assisted anesthesia systems that can provide more comfortable injections. Some dentists offer pre-injection topical anesthetics to numb the area first. Relaxation techniques, such as deep breathing or listening to music, may also help manage anxiety.