If you buy through links on our site, we may earn a small affiliate commission to help support the blog - at no extra cost to you. It never influences our product selection process. Thank you!
Is your CPAP machine secretly damaging your dental health? You’re not alone. Many sleep apnea sufferers discover that while their breathing improves at night, their teeth may be paying the price.
When you use a CPAP machine to manage sleep apnea, the constant air pressure can create unexpected side effects for your teeth and gums. From shifting tooth alignment to increasing dryness in your mouth, these oral health complications often go undiscussed during initial CPAP therapy conversations. Understanding the connection between your CPAP treatment and dental problems is the first step toward protecting both your sleep quality and your smile.
Understanding CPAP Therapy and Dental Health
CPAP therapy works by delivering a continuous stream of air through a mask worn over your nose or mouth while sleeping. This positive airway pressure keeps your airways open, preventing the breathing interruptions characteristic of sleep apnea. Many CPAP users experience important improvements in their sleep quality, daytime alertness, and overall health.
Even though these benefits, CPAP therapy can inadvertently affect your dental health in several ways. The mask’s positioning and pressure often create forces that gradually shift teeth over time. Dental changes typically occur slowly, sometimes taking months or years before becoming noticeable.
“I noticed my bite felt different about a year after starting CPAP therapy,” shares Michael, a long-term CPAP user. “My front teeth no longer aligned properly when I closed my mouth, and I started experiencing jaw pain that wasn’t there before.”
Dr. Todd B. Harris points out that “Many patients come to me confused about their changing dental alignment, unaware that their nightly CPAP use might be contributing to these shifts. The consistent pressure from mask straps and the position required for effective therapy creates subtle but important forces on dental structures.”
CPAP-related dental issues aren’t limited to tooth alignment. The therapy often leads to decreased saliva production and chronic dry mouth. This reduction in saliva creates an environment where bacteria thrive, increasing your risk for cavities, gum disease, and halitosis. Properly fitted masks and regular dental check-ups are essential for minimizing these potential complications.
How CPAP Therapy Can Affect Your Teeth

CPAP therapy effectively treats sleep apnea but can impact your dental health in several ways. Research shows that long-term use of CPAP machines may lead to dental problems that aren’t immediately obvious until they become more severe.
Jaw Misalignment and Tooth Movement
The positive airway pressure from CPAP therapy can gradually push against your teeth, causing them to shift from their original position. These shifts often lead to changes in your bite pattern and jaw alignment, potentially resulting in tooth pain and discomfort. Studies indicate that the continuous pressure from nightly CPAP use affects dental occlusion similarly to mandibular advancement devices, with a noticeable decrease in occlusal contact points in the molar region.
One patient, Sarah, shared her experience: “After using my CPAP for three years, I noticed my front teeth weren’t lining up correctly anymore. My dentist confirmed that my bite had changed, and we traced it back to my CPAP use. I had no idea this could happen.”
Dry Mouth and Increased Cavity Risk
CPAP therapy frequently causes xerostomia (dry mouth) because you’re more likely to breathe through your mouth during sleep. This reduced saliva production disrupts your mouth’s natural pH balance, creating an environment where cavity-causing bacteria thrive. Saliva plays a crucial role in neutralizing acids and remineralizing teeth, so its reduction significantly increases your risk of tooth decay.
The combination of dry mouth and altered bacterial environment can accelerate cavity formation even if you’ve previously had good dental health. Regular dental check-ups become especially important for CPAP users to catch these issues early before they develop into more serious problems.
Common Dental Issues Reported by CPAP Users

CPAP therapy effectively treats obstructive sleep apnea but can introduce several oral health challenges that impact your dental wellbeing. Many CPAP users report similar dental problems that develop gradually after beginning their therapy.
Bite Changes and Orthodontic Concerns
Long-term CPAP use often causes teeth to shift position, leading to malocclusion or bite misalignment issues. Your jaw position may change over time as the continuous pressure from the CPAP device pushes against your teeth and oral structures. These alterations can affect your facial structure and potentially worsen sleep apnea by narrowing the airway when your lower jaw shifts backward.
“After using my CPAP for five years, I noticed my front teeth weren’t lining up properly anymore,” shares Michael, a 52-year-old CPAP user. “My dentist confirmed the pressure from my mask had gradually changed my bite alignment.”
Many users require orthodontic intervention, including retainers, to correct these CPAP-induced dental shifts. The bite changes frequently cause chronic headaches and pain in the neck and back due to abnormal jaw alignment. Regular dental monitoring helps identify these changes early before they become important problems requiring extensive correction.
Morning Jaw Pain and TMJ Problems
Temporomandibular joint disorders (TMD) commonly develop in CPAP users who experience morning jaw discomfort. The continuous pressure from your CPAP device can trigger or worsen tooth grinding (bruxism) and clenching during sleep. These unconscious behaviors place additional stress on your temporomandibular joints, resulting in pain and dysfunction.
Signs of TMJ problems include clicking sounds when opening your mouth, limited jaw movement, and facial pain radiating from the jaw joint. The damage to your temporomandibular joints from CPAP-related pressure can contribute to longer-term jaw dysfunction and persistent discomfort.
Dr. Harris notes, “Many of my patients using CPAP therapy don’t connect their morning jaw pain with their sleep apnea treatment. The relationship between CPAP use and TMJ issues requires attention from both sleep specialists and dental professionals to manage effectively.”
CPAP users experiencing jaw pain should consider using a mouth guard alongside their therapy to protect against grinding and clenching behaviors. Adjusting your mask fit and pressure settings might also reduce jaw strain while maintaining effective sleep apnea treatment.
Signs Your CPAP Might Be Damaging Your Teeth

Persistent Dry Mouth
Dry mouth, or xerostomia, serves as a primary indicator that your CPAP therapy might be affecting your dental health. Air leaks from an improperly fitted mask reduce saliva production during sleep, creating an environment where harmful bacteria thrive. Many patients report waking up with an uncomfortably parched mouth even though using a CPAP humidifier.
“I’ve been using my CPAP for three years and constantly battled dry mouth,” shares Rebecca, a patient at our clinic. “I didn’t realize this dryness was actually putting my teeth at risk until my dentist pointed out early signs of decay at my check-up.”
Increased Tooth Sensitivity
Your teeth might signal CPAP-related damage through heightened sensitivity to hot, cold, or sweet foods. This sensitivity often stems from enamel erosion caused by reduced saliva flow and increased acidity in your mouth during CPAP use. Morning discomfort when brushing or eating breakfast frequently indicates potential issues with your therapy’s impact on dental health.
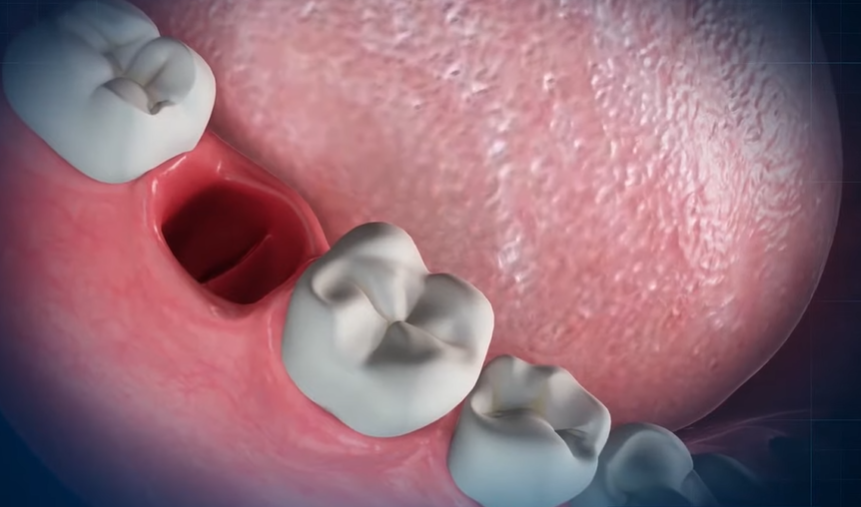
Visible Shifting of Teeth
CPAP therapy applies continuous positive pressure that can physically move your teeth over time. You might notice new gaps between teeth, changes in how your bite feels, or front teeth that appear more protruded than before. These changes typically develop gradually, becoming apparent only after months or years of consistent CPAP use.
Worsening Tooth Decay
The combination of dry mouth and decreased protective saliva creates perfect conditions for accelerated tooth decay. You may experience more cavities than usual even though maintaining your regular oral hygiene routine. Cavity formation concentrated near the front teeth often indicates CPAP-related issues rather than typical decay patterns.
Jaw Pain and Discomfort
Morning jaw soreness might indicate that your CPAP therapy is affecting your dental alignment. The pressure from CPAP can cause unconscious clenching or grinding during sleep as your jaw muscles respond to the airflow forces. Clicking sounds when opening your mouth, limited jaw movement, and facial pain represent classic signs of CPAP-induced temporomandibular joint problems.
Changes in Bite Alignment
Your bite may feel “off” when chewing, with teeth not meeting as they once did. This malocclusion often results from gradual tooth movement caused by CPAP pressure. Many patients describe this sensation as teeth suddenly feeling like they “don’t fit together properly” even though no recent dental work.
Prevention Strategies to Protect Your Dental Health

Protecting your dental health while using CPAP therapy requires proactive measures and regular maintenance. These strategies help minimize the risk of tooth decay, movement, and other oral health complications associated with CPAP use.
CPAP Mask Adjustments and Alternatives
Proper mask fitting serves as the foundation for preventing dental problems with CPAP therapy. Correctly fitted masks significantly reduce air leakage around the mouth, which decreases dryness and subsequent dental issues. Many patients find that nasal pillows or full-face masks better limit mouth breathing compared to other options, helping maintain normal saliva production throughout the night.
Dr. Todd B. Harris often recommends considering oral appliance therapy as an alternative for patients experiencing dental complications from CPAP. “I’ve seen remarkable improvements in patients who switched to oral appliances,” Dr. Harris notes. “Unlike CPAP, these devices don’t create the positive pressure that can push teeth forward, substantially reducing the risk of tooth movement and jaw alignment issues.”
Adjusting your CPAP humidification settings can also make a important difference in preventing dry mouth. Higher humidity levels keep oral tissues moistened, countering the drying effect of constant airflow. Testing different mask types during a fitting session with your sleep specialist ensures you find the option that creates the fewest dental side effects while effectively treating your sleep apnea.
Dental Interventions and Treatments
Regular orthodontic monitoring becomes essential for long-term CPAP users experiencing tooth shifting or flaring. Orthodontists can provide interventions such as retainers or alignment correction treatments to address changes caused by sustained CPAP pressure. Retention devices worn during non-CPAP hours help maintain proper tooth position and prevent further movement.
Treatment approaches for dry mouth include prescription-strength fluoride toothpaste, specially formulated mouth rinses, and saliva substitutes. Jennifer, a 5-year CPAP user, shares, “My dentist recommended a xylitol-based mouth spray that I use before bed, and it’s dramatically reduced my dry mouth symptoms and subsequent cavity formation.”
Professional management of tooth sensitivity and decay requires prompt attention to emerging issues. CPAP users benefit from more frequent dental evaluations—typically every 4 months rather than the standard 6-month interval—to detect early signs of enamel erosion or movement. Dentists may apply specialized varnishes or sealants to protect vulnerable tooth surfaces from the effects of reduced saliva and increased acidity.
Maintaining excellent oral hygiene practices remains crucial while using CPAP therapy. Brushing thoroughly twice daily with fluoride toothpaste, flossing daily, and using an alcohol-free mouth rinse help combat the increased risk of bacterial growth. Staying well-hydrated throughout the day by drinking at least 8 glasses of water supplements your body’s ability to produce saliva, creating natural protection against the drying effects of CPAP treatment.
Working With Healthcare Providers for Solutions

Regular dental check-ups become essential when you’re using CPAP therapy to monitor any early signs of tooth decay or gum disease. Your dentist can spot potential issues before they worsen and recommend personalized interventions based on your exact situation. Dr. Todd B. Harris suggests, “CPAP users should visit their dentist quarterly rather than biannually to catch dental changes early.”
Addressing dry mouth remains a primary concern for many CPAP users. Healthcare providers frequently recommend integrated humidifiers for CPAP machines to maintain oral moisture levels throughout the night. Specialized saliva substitutes and alcohol-free mouthwashes can provide additional protection against the drying effects of continuous airflow.
Oral appliance therapy offers an alternative for patients experiencing important dental issues from CPAP use. These custom-fitted devices reposition the jaw and tongue to maintain an open airway without the problematic air pressure that affects tooth positioning. Jennifer, a long-term CPAP user who switched to an oral appliance, shares, “After noticing my teeth shifting, my sleep specialist recommended an oral appliance. Within months, not only did my sleep apnea symptoms remain controlled, but my dental discomfort disappeared completely.”
Customized mask fitting dramatically reduces air leakage that contributes to dry mouth and subsequent dental problems. Working with your sleep specialist to find the ideal mask style and size for your facial structure can minimize these issues. Full-face masks might reduce mouth breathing for some patients, while nasal masks with chin straps help others keep their mouths closed during sleep.
Collaborative care between your sleep specialist and dentist creates the most effective treatment plan for managing both sleep apnea and dental health. Share your dental concerns with your sleep doctor and inform your dentist about your CPAP therapy to ensure both professionals understand the complete picture of your health needs. This team approach allows for adjustments to your therapy that preserve dental integrity while maintaining effective sleep apnea treatment.
Conclusion
Your dental health doesn’t need to suffer because of your CPAP therapy. By recognizing the potential issues early and taking proactive steps you can protect your teeth while still getting the sleep apnea treatment you need.
Work closely with both your dentist and sleep specialist to create a personalized approach that addresses your exact concerns. Regular dental monitoring combined with proper mask fitting and humidity adjustments can make a important difference.
Don’t hesitate to explore alternatives like oral appliances if CPAP is causing persistent dental problems. Remember that treating your sleep apnea and maintaining dental health aren’t mutually exclusive goals – with the right approach you can successfully manage both.
Frequently Asked Questions
Can CPAP therapy affect my dental health?
Yes, CPAP therapy can impact your dental health. While improving your sleep and overall health, it may cause tooth shifting, dry mouth, and jaw misalignment over time. The mask’s positioning and pressure can gradually move teeth, often unnoticed until significant changes occur. These effects vary among users but are important to monitor.
What are the common dental issues CPAP users experience?
Common dental issues include bite changes, tooth shifting, increased cavity risk, dry mouth, jaw pain, and temporomandibular joint (TMJ) problems. Long-term use can lead to malocclusion (misaligned teeth) and changes in jaw position. Some users report morning jaw pain from unconscious tooth grinding and clenching triggered by the CPAP pressure.
How does CPAP therapy cause dry mouth?
CPAP therapy can decrease saliva production and cause air leaks from improperly fitted masks, leading to dry mouth. This creates an environment where cavity-causing bacteria thrive due to disrupted pH balance. Reduced saliva also means less natural cleaning action in your mouth, increasing risks of cavities, gum disease, and bad breath.
What signs indicate CPAP is damaging my dental health?
Watch for persistent dry mouth, increased tooth sensitivity, visible shifting of teeth, worsening tooth decay, jaw pain, and changes in bite alignment. If you notice your teeth don’t fit together as they used to, experience new discomfort when chewing, or develop persistent morning headaches, consult your dentist promptly.
How can I prevent dental problems while using CPAP?
Prevent dental issues by ensuring proper mask fitting to reduce air leakage, adjusting humidification settings, maintaining excellent oral hygiene, staying hydrated, and using a mouth guard if you grind your teeth. Consider alternative therapies like oral appliances if problems persist. Most importantly, schedule regular dental check-ups (quarterly rather than biannually) to catch problems early.
Should I tell my dentist about my CPAP use?
Absolutely. Inform your dentist about your CPAP therapy so they can monitor for specific issues and recommend preventive measures. Collaborative care between your sleep specialist and dentist creates the most effective treatment plan that addresses both sleep apnea and dental health. This team approach ensures comprehensive care tailored to your needs.
Are there alternatives to CPAP that won’t affect my teeth?
Yes, oral appliance therapy is an alternative for those experiencing significant dental issues from CPAP use. These custom-fitted devices reposition the jaw to keep airways open without the pressure that shifts teeth. For some patients, positional therapy, weight management, or surgical options may also be appropriate alternatives, depending on sleep apnea severity.
How often should CPAP users visit the dentist?
CPAP users should consider quarterly dental visits instead of the standard biannual schedule. This increased frequency allows dentists to catch early signs of tooth decay, gum disease, or alignment changes before they become serious problems. Regular professional cleanings are also essential to combat the increased risks associated with dry mouth.