If you buy through links on our site, we may earn a small affiliate commission to help support the blog - at no extra cost to you. It never influences our product selection process. Thank you!
Many people worry about what happens if their dental implant causes pain or doesn’t fit right. It’s natural to wonder if these implants can be removed easily, especially since they’re meant to last a long time.
Yes, dental implants can be removed—but the process is often complex because the implant is firmly attached to the jawbone.
This doesn’t mean implants are a bad choice. Knowing they can be taken out if needed can give patients peace of mind. Removal usually requires a dental professional and careful planning to protect the surrounding bone and tissues.
This article will explain why implants might need removing, how the process works, recovery expectations, and what comes next. Understanding these details helps people make better decisions about their dental health.
Yes, But It’s Not Simple

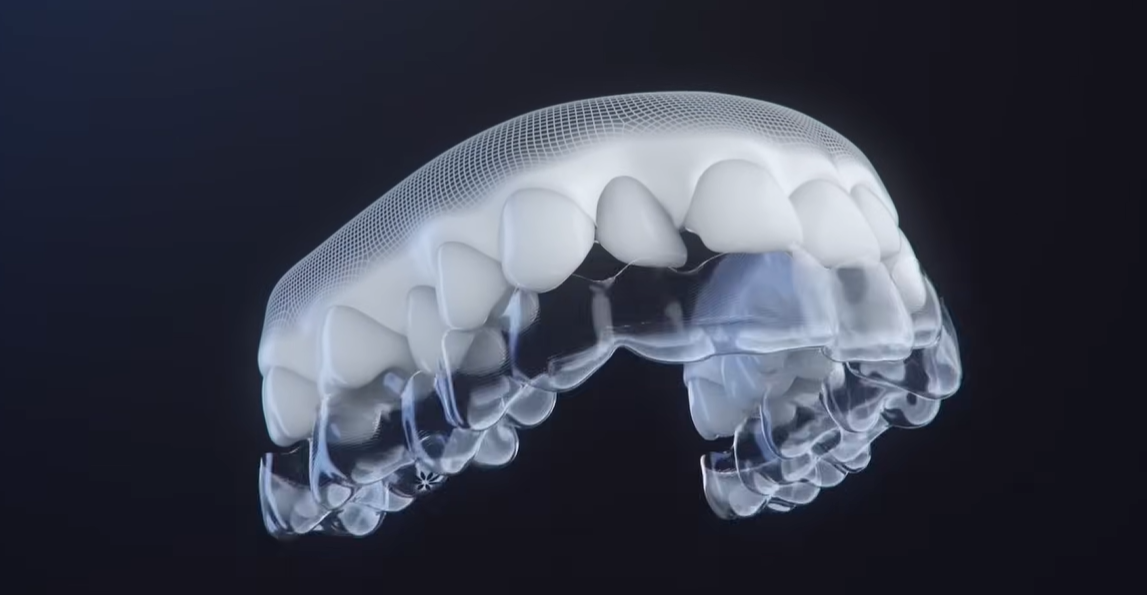
Dental implants can be removed, but it’s not a simple process. Unlike natural teeth, implants are designed to fuse tightly with the jawbone. This process, called osseointegration, means the bone grows directly around the implant, making it very secure.
Because of this bond, removing an implant is more challenging than pulling out a loose tooth. Dr. Todd B. Harris, DDS, Prosthodontist at Harris Dental Associates, explains: “Once osseointegration occurs, the implant is nearly fixed to the bone. Removal requires careful techniques to avoid damaging the surrounding bone.”
The difficulty matters because the surgeon must protect the bone so the area can heal properly. Damaging the bone can lead to longer recovery times or complicate future implant procedures.
In short, while dental implants can be removed, their integrated nature makes removal a precise task. Patients should expect a professional evaluation and possibly advanced surgical care to remove implants safely.
When and Why Implant Removal Becomes Necessary
Dental implants are built to last, but sometimes removal is necessary. The reasons usually involve infection, failed bonding with the bone, or healing problems.
Infection (Peri-Implantitis) is one common cause. Michael, 47, experienced swelling and pain around his implant. The infection spread, making it impossible to save the implant. In such cases, removal stops the infection from damaging nearby bone and tissue. Early signs include redness, bleeding, and discomfort. Preventing this requires good oral hygiene and regular dental check-ups.
Failed Osseointegration is another reason. Sarah’s implant felt loose after three years. This failure means the implant can’t support a crown or denture properly. Without solid integration, chewing might become painful, and the implant can move. Causes include poor bone quality, smoking, or medical conditions. Removal is needed to avoid further bone loss.
Poor healing or other complications can also require removal. Some patients face issues like bone loss, implant breakage, or allergic reactions. These problems may cause pain or prevent normal function. If a complication makes the implant unstable or uncomfortable, removing it is the safest choice.
| Reason | Symptoms | Why Removal Needed | Prevention |
|---|---|---|---|
| Infection (Peri-Implantitis) | Swelling, redness, pain | Stop infection spreading | Good hygiene, dental check-ups |
| Failed Osseointegration | Loose implant, pain | Implant can’t support chewing | Careful patient selection, no smoking |
| Poor Healing / Complications | Pain, bone loss, instability | Avoid further damage | Follow post-surgery guidance |
Removing an implant is sometimes necessary to maintain oral health and prepare for future treatment. Knowing these reasons helps patients and dentists make informed decisions.
How the Removal Process Works
Removing dental implants is a careful, step-by-step process that requires skill and precision.
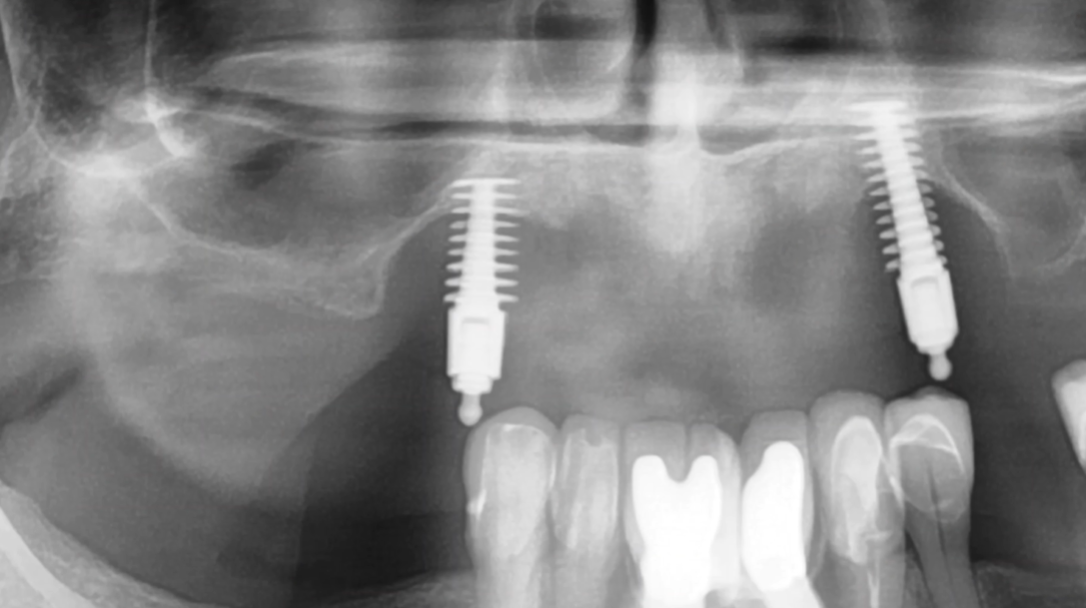
First comes evaluation, which often includes a CBCT scan. This scan helps the dentist see the implant’s position and bone condition. Dr. Harris emphasizes that this step is crucial to plan the removal safely and avoid damage to surrounding tissues.
Next, anesthesia is administered to reduce pain and discomfort. Local anesthesia or sedation may be used depending on the case.
The surgeon then accesses the implant by making a small incision in the gums to expose the implant and bone.
After gaining access, the implant is carefully loosened. This is done with controlled force to reduce bone loss and avoid damage. Once loose, the implant is gently removed from the jaw.
Site cleanup follows, removing any infected tissue or debris to promote healing and prepare the area—especially if a replacement implant is planned.
Finally, the site is closed with stitches. Proper closure helps reduce infection risk and speeds recovery.
This process shows that while dental implants can be removed, the procedure is complex. Only a trained specialist should perform it with careful planning.
Removal Techniques and Tools
Removing dental implants requires the right tools and techniques to protect the surrounding bone and tissue. The choice depends on how well the implant has fused with the bone.
Simple mechanical removal works when the implant is loose or failing. The dentist can unscrew the implant using standard tools without much damage.
For well-integrated implants, a trephine burr is often used. This specialized cutting tool removes a small ring of bone around the implant. Dr. Harris notes: “The trephine burr allows for careful bone removal, minimizing trauma while freeing the implant.” This technique requires precision to avoid removing too much bone—essential if future implant replacement is planned.
Reverse torque applies controlled counterclockwise force to unscrew the implant. This technique works best when the implant is stable but needs removal. The force must be carefully applied to avoid fracturing the implant or damaging bone.
Ultrasonic devices are also used. These tools vibrate gently to loosen the implant from bone, reducing pressure and heat buildup while preserving surrounding tissue.
Using these methods requires skill and experience. Removing implants improperly can harm nearby teeth and nerves. Expert dentists assess bone health and choose the safest approach, balancing effective removal with preserving bone for future dental work.
Is Implant Removal Painful?
Removing dental implants is usually not painful during the procedure. Dentists use local anesthesia to numb the area, so patients mostly feel pressure and vibrations—not pain.
Before the procedure, dentists often offer anti-anxiety options to help calm nerves. These can include mild sedatives or breathing techniques to ease stress. This helps make the experience smoother, especially for those worried about discomfort.
After the implant is removed, mild soreness and swelling are common. This soreness can last a few days but is generally manageable with proper care. Patients often use prescribed pain medications or over-the-counter painkillers as advised.
Jennifer, who once feared implant removal, shared that her worry was worse than the procedure itself. “I felt only slight pressure during removal,” she said, “and my recovery was quick with the right pain management.”
To reduce discomfort after surgery:
-
Use ice packs 20 minutes on, 20 off
-
Take prescribed pain medications as directed
-
Sleep with your head elevated
-
Stick to soft foods for the first week
-
Avoid straws and hot beverages
Following these steps helps control swelling and soreness. Most people find that straightforward care keeps pain at a low, manageable level.
Recovery Timeline and What to Expect
Recovery after implant removal varies by individual, but here’s what to typically expect:
First 24 Hours: Bite down on gauze to stop bleeding. Some oozing is normal. Rest and avoid strenuous activity. Pain meds should keep discomfort minimal.
Week 1: Stitches typically come out around day 7. Swelling peaks around days 2-3, then decreases. Bruising may appear—this is normal and will fade. Continue soft foods and gentle rinsing with salt water (not in first 24 hours).
Weeks 2-4: Swelling resolves and stitches come out. You can gradually return to a normal diet, though you should still avoid hard or crunchy foods. Gum healing is underway, and you can resume normal activities.
Months 1-3: Complete gum healing occurs. Bone starts adapting. If a bone graft was placed, integration begins. Full recovery is typically complete by 3 months.
Red Flags—When to Contact Your Dentist:
-
Excessive bleeding that won’t stop
-
Severe pain increasing after day 3
-
Swelling getting worse after day 3
-
Signs of infection (fever, pus, warmth)
-
Dry socket symptoms (extreme pain)
Early intervention can prevent complications, so don’t hesitate to call if something doesn’t feel right.
Can You Get a New Implant After Removal?
Yes—usually you can get another implant, but timing matters. Your dentist will need to assess bone quality and healing before placing a replacement.
Typical waiting period: 3-6 months for bone to adapt and recover. If bone was removed during extraction, regrowth is needed. If infection caused removal, it must fully clear first.
After waiting: Your dentist re-evaluates bone with CBCT scanning. If bone volume and quality are good, a new implant can often be placed successfully.
If bone isn’t sufficient: A bone graft may be needed first, which requires another 3-6 month healing period before implant placement.
Success rates: Second implants have very high success rates—around 95%—similar to first implants. Good planning ensures success.
Sarah’s experience illustrates this well. After her first implant failed, Dr. Harris recommended waiting 4 months for bone recovery. “Then he placed a new implant,” Sarah shared. “This time I’m religious about care. The new implant feels stable and looks great.”
Prevention: Protecting Your Implant Long-Term
Most implant removals are preventable with proper care. Here’s how to protect your implant:
Excellent oral hygiene is most important. Brush twice daily with a soft brush, floss daily, and pay special attention to the implant area.
Regular professional checkups—every 6 months—let Dr. Harris catch problems early. Early intervention prevents removal and keeps your implant healthy.
Avoid harmful habits: No smoking (worsens gum disease), no chewing ice or hard objects, and no grinding teeth (wear a night guard if needed).
Manage medical conditions: Diabetes, gum disease, and autoimmune conditions increase infection risk. Keep them controlled and communicate with your dentist.
Monitor your implant: Know what “normal” feels like and alert your dentist to any changes. Watch for swelling, pain, movement, or bleeding.
Dr. Harris emphasizes: “The best implant removal is the one that never happens. With good oral care, regular checkups, and early intervention when problems appear, most implants last a lifetime.”
FAQ: Your Questions About Implant Removal Answered
How much does dental implant removal cost?
Costs vary from $500-$2,500 depending on complexity. Loose implants cost less; well-integrated ones more. Check with your provider—many insurance plans cover medically necessary removal.
Does implant removal leave a hole in your jaw?
Physically yes, but appearance-wise no. The gum closes over the socket and bone gradually fills in. You won’t notice anything, and others won’t either.
Is implant removal an emergency?
Usually not. Most cases can be scheduled. Exception: If you have severe infection with fever or significant swelling, contact your dentist immediately.
How long does implant removal take?
Loose implants: 15-30 minutes. Well-integrated: 30-60 minutes. Complex cases: up to 90 minutes. Most are under 1 hour total.
Can I eat right after removal?
Not the same day. First 24 hours: soft, cool foods only. Gradually return to normal diet by week 2. Avoid hot foods in the first week.
When to Contact Harris Dental Associates
Contact if:
-
You’re worried about your implant
-
You notice any warning signs
-
You want to prevent problems
-
You’re considering removal options
-
You want to discuss replacement options
Call immediately if:
-
You have severe pain not controlled by medication
-
You have significant swelling or fever
-
Your implant appears to be moving
-
You have severe bleeding that won’t stop
What to expect at consultation:
-
Full implant evaluation
-
Assessment of your concerns
-
Discussion of your options
-
3D imaging if needed
-
Honest recommendation
-
Personalized treatment plan
📞 Your Implant Health Matters: Expert Care When You Need It
Your implant is a valuable investment in your smile. At Harris Dental Associates, Dr. Todd B. Harris specializes in implant care, complications, and solutions.
Whether you’re concerned about an existing implant, considering removal, or planning replacement options, we’re here to help with:
-
Expert evaluation and assessment
-
Honest discussion of all options
-
Compassionate, patient-first care
-
Latest technology and techniques
-
Clear communication throughout
Don’t wait if you’re worried about your implant. Schedule your consultation with Dr. Harris today.
Schedule Your Consultation
Call: (508) 584-6070