If you buy through links on our site, we may earn a small affiliate commission to help support the blog - at no extra cost to you. It never influences our product selection process. Thank you!
Are you experiencing severe tooth pain that just won’t go away? An example of endodontic treatment is a root canal—a procedure that saves your natural tooth by removing infected pulp and preventing further damage.
When infection reaches the inner chambers of your tooth, only specialized dental care can address the problem. Endodontic treatments focus on the dental pulp and tissues surrounding the tooth roots. Even though their intimidating reputation, modern root canal procedures are relatively comfortable and provide immediate relief from the throbbing pain of dental infections.
Understanding Endodontic Treatment: What It Is and Why It’s Needed
Endodontic treatment focuses on the dental pulp and tissues surrounding the roots of teeth. This specialized dental procedure addresses infections and damage inside teeth, particularly in the pulp chamber and root canals. Most commonly, endodontic treatment is referred to as a root canal procedure, though this term technically describes just one aspect of endodontic care.
Root canal therapy becomes necessary when bacteria invade the pulp chamber of your tooth due to deep decay, repeated dental procedures, cracks, or traumatic injuries. The infected pulp tissue, containing nerves and blood vessels, causes important pain and can lead to abscess formation if left untreated. Dr. Todd B. Harris explains, “I’ve seen patients who’ve endured weeks of excruciating pain before seeking treatment, not realizing that endodontic therapy could provide immediate relief.”
One patient, Sarah, described her experience: “I’d been taking pain relievers for months, thinking my toothache would eventually go away. When Dr. Harris diagnosed the infection and performed the root canal, I couldn’t believe how quickly the pain disappeared. I wish I hadn’t waited so long!”
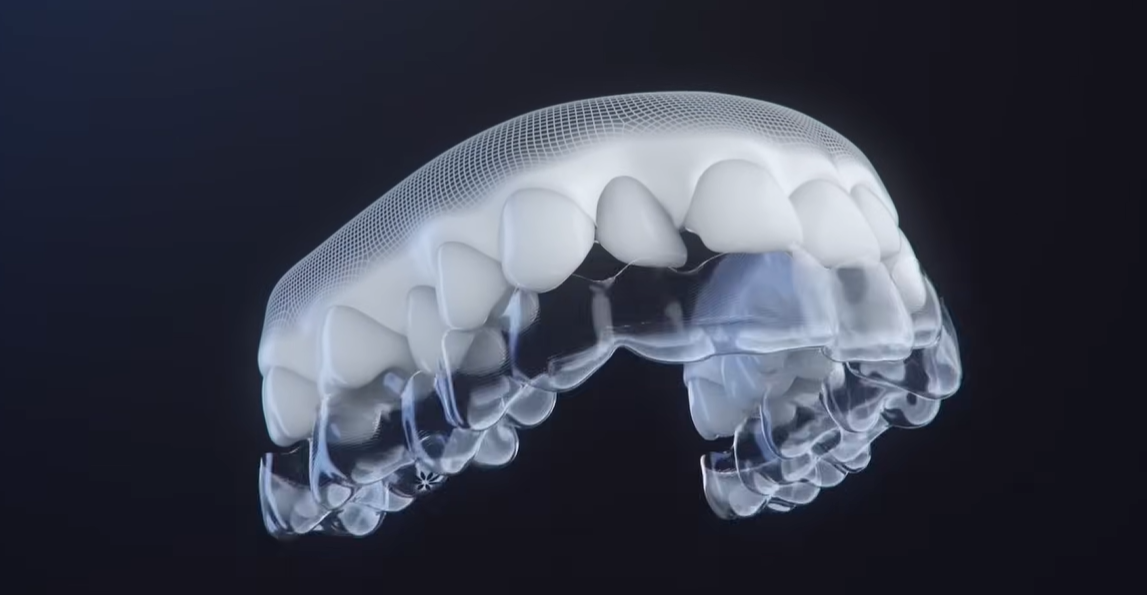
The primary goal of endodontic treatment is preserving your natural tooth rather than extracting it. During the procedure, the dentist removes the infected pulp, cleans and shapes the root canals, then seals them to prevent future infections. Modern endodontic techniques employ advanced technology such as digital imaging, specialized microscopes, and improved anesthetic methods that make the procedure more comfortable than ever before.
Saving your natural tooth through endodontic treatment offers several advantages over extraction: maintaining normal biting force, efficient chewing, natural appearance, protection of other teeth from excessive strain, and prevention of costly dental implants or bridges. The success rate for endodontic procedures exceeds 95% with proper care, and most treated teeth last a lifetime.
Root Canal Therapy: The Classic Example of Endodontic Treatment

Root canal treatment represents the most common endodontic procedure performed today. This therapy involves removing infected or inflamed pulp from inside a tooth to preserve the natural tooth structure and prevent extraction. By targeting the source of dental pain and infection, root canal therapy provides both immediate relief and long-term tooth preservation.
The Step-by-Step Process of Root Canal Treatment
The root canal procedure follows a systematic approach to effectively eliminate infection and restore tooth function. Your endodontist begins with a thorough diagnosis using clinical examination and dental X-rays to confirm pulp damage or infection. Local anesthesia ensures you remain comfortable throughout the entire procedure, eliminating the pain many patients fear.
After creating a small access opening in the crown of your tooth, the specialist uses specialized instruments to remove the infected pulp, carefully shaping the canals while cleaning out harmful bacteria and debris. The empty canals are then filled with a biocompatible material called gutta-percha along with adhesive cement to seal the space completely and prevent any future reinfection.
A temporary filling closes the access hole initially, which your dentist later replaces with a permanent restoration. The final step typically involves placing a crown or other restoration to protect the treated tooth and restore full functionality.
“Many patients come to me thinking they need an extraction, but are relieved to learn a root canal can save their natural tooth,” explains Dr. Todd B. Harris. “One patient, Michael, had been suffering from severe tooth pain for weeks before visiting our office. After his root canal treatment, he called the next day amazed at how quickly his pain had disappeared and how straightforward the procedure had been.”
Modern Technologies Improving Root Canal Procedures
Today’s root canal treatments have evolved dramatically thanks to technological advancements. Digital X-rays provide clearer, more detailed images with significantly less radiation exposure than traditional films. Microscopic instruments allow for more precise cleaning and shaping of even the smallest canals.
Advanced irrigation techniques using ultrasonic activation ensure thorough disinfection of the entire canal system. Biocompatible filling materials have improved dramatically, creating better seals and reducing the risk of future complications.
These innovations have transformed root canals into quicker, more comfortable procedures that can often be completed in just one or two visits. Recovery time has decreased substantially, with most patients returning to normal activities within 24 hours of treatment.
The success rate of modern root canal therapy exceeds 95%, making it an extremely reliable option for saving damaged teeth. Digital treatment planning helps endodontists visualize the entire procedure beforehand, eliminating surprises and ensuring optimal outcomes for every patient.
Pulpotomy: A Partial Endodontic Treatment Option

A pulpotomy represents a less invasive alternative to a full root canal, involving the removal of infected pulp only from the crown portion of the tooth while preserving the healthy pulp in the roots. This partial endodontic procedure serves as an effective treatment option for exact dental conditions, particularly in primary teeth.
When Pulpotomy Is Recommended Over Complete Root Canal
Dentists recommend pulpotomies primarily for primary (baby) teeth with extensive decay but no infection in the roots or surrounding bone. These procedures are ideal when the pulp exposure results from deep cavities or trauma, but the infection remains confined to the crown pulp. Unlike complete root canal treatment that removes all pulp tissue from both crown and roots, pulpotomies maintain the vitality of the remaining pulp tissue.
Dr. Todd B. Harris explains, “Many parents panic when they hear their child needs endodontic treatment, but a pulpotomy is often the perfect solution for saving a baby tooth while being less traumatic than a full root canal.”
The procedure typically involves removing damaged pulp from the crown, applying a medicated dressing to protect remaining healthy tissue, and then sealing the tooth with a restoration. Commonly referred to as a “baby root canal,” this treatment preserves tooth function until the primary tooth naturally falls out.
One patient, Michael, brought his 6-year-old daughter in with severe tooth pain. “I was relieved when Dr. Harris suggested a pulpotomy instead of extraction,” Michael shares. “The procedure was quick, and my daughter was pain-free that same day. Her tooth remained healthy until it naturally fell out years later.”
For permanent teeth, pulpotomies may occasionally be performed on young teeth with immature roots or as an emergency procedure until a complete root canal can be scheduled. The preservation of vital pulp tissue makes pulpotomy a valuable option in the endodontic treatment arsenal, offering a less invasive path to dental health.
Apicoectomy: Surgical Endodontic Treatment
An apicoectomy is an advanced surgical endodontic procedure performed when conventional root canal therapy fails or can’t be redone successfully. This specialized treatment, also known as root-end surgery or retrograde root canal treatment, serves as a last effort to save a tooth that might otherwise require extraction.
What is an Apicoectomy?
Apicoectomy procedures involve the surgical removal of the tooth root’s tip (apex). During this microsurgical treatment, the dentist removes the infected root tip and prepares a small cavity at the end of the root canal. This cavity is then sealed with biocompatible materials to prevent reinfection and promote healing. The procedure specifically targets persistent infections located at the root tip that remain beyond the reach of traditional root canal cleaning methods.
When is an Apicoectomy Needed?
Apicoectomies become necessary in several exact situations. Persistent infection following a conventional root canal treatment often indicates the need for this procedure. Anatomical complexities that prevent complete cleaning through standard methods may also necessitate an apicoectomy. Cases where retreatment isn’t possible or has been unsuccessful commonly lead to this surgical approach. Removing the root tip allows dentists to eliminate infected tissue that couldn’t be cleaned during previous treatments.
Dr. Todd B. Harris notes, “Many patients are relieved to learn there’s still a way to save their natural tooth even after a root canal has failed. Apicoectomies offer that second chance at preservation before considering extraction.”
Procedure and Techniques
Modern apicoectomy techniques use advanced microsurgical approaches for enhanced precision and outcomes. Dental operating microscopes provide magnification that allows for extremely detailed work at the root tip. Ultrasonic instruments create more conservative and precise root-end preparations than traditional drilling methods. Advanced sealing materials, particularly calcium-silicate-based fillings, offer superior biocompatibility and sealing ability compared to earlier materials.
The procedure typically begins with a small incision in the gum tissue to expose the underlying bone and root. After accessing the root tip, the dentist removes the infected tissue along with a small portion of the root end. Special instruments then prepare a small cavity in the remaining root end, which is filled with biocompatible sealing material before the gum tissue is sutured back in place.
Recovery and Success Rates of Apicoectomy
Apicoectomy recovery typically progresses smoothly for most patients with minimal downtime. Mild discomfort and swelling may occur during the first 24-48 hours following the procedure. Cold compresses and prescribed pain medications effectively manage these temporary symptoms. Most patients return to normal activities within 2-3 days after surgery.
Success rates for apicoectomies are remarkably high, ranging between 85-95% depending on case complexity. Proper case selection significantly influences outcomes, with better results in teeth without severe periodontal disease. Follow-up appointments ensure proper healing and monitor the long-term success of the procedure.
One of Dr. Harris’s patients, Michael, shares his experience: “After two failed root canals on the same tooth, I was convinced extraction was my only option. The apicoectomy Dr. Harris performed saved my tooth, and the recovery was much easier than I expected. Five years later, that tooth is still perfectly functional.”
For cases where apicoectomy isn’t viable, alternatives include extraction followed by prosthetic replacement options such as dental implants, bridges, or removable dentures. But, preserving the natural tooth through apicoectomy offers important advantages in maintaining normal bite function and jaw structure when possible.
Pain Management During and After Endodontic Procedures

Effective pain control stands as a cornerstone of successful endodontic treatment, ensuring your comfort throughout the procedure and recovery process. Modern endodontic practices employ multiple strategies to minimize discomfort at every stage of treatment.
Local Anesthetic Techniques
Local anesthetics provide immediate numbing of the treatment area, eliminating pain during the procedure. Standard injections effectively block sensation in most cases, while specialized techniques address more challenging situations. Advanced methods like periodontal ligament (PDL) injections and Gow-Gates nerve blocks prove particularly valuable for difficult-to-anesthetize teeth such as mandibular molars. These techniques ensure you’ll remain comfortable even during complex root canal procedures.
“Many patients express surprise at how painless their root canal experience was,” notes Dr. Todd B. Harris. “With today’s advanced anesthetic techniques, we’re able to ensure complete comfort even in cases where traditional numbing methods might have been less effective.”
Pharmacological Approaches
Medications play a crucial role in managing pain before, during, and after endodontic treatment. A combined approach using different analgesics often provides superior relief:
| Medication Type | Examples | Primary Benefits |
|---|---|---|
| NSAIDs | Ibuprofen | Reduces inflammation and pain |
| Acetaminophen | Tylenol | Enhances pain relief when combined with NSAIDs |
| Long-acting anesthetics | Bupivacaine | Extends pain relief after treatment |
| Corticosteroids | Dexamethasone | Manages flare-ups and reduces inflammation |
Lisa, a recent patient, shares her experience: “I’d been terrified of root canal pain based on stories I’d heard, but Dr. Harris prescribed a combination of ibuprofen and acetaminophen that kept me comfortable throughout recovery. I felt almost no pain after the procedure.”
Non-Pharmacological Strategies
Beyond medications, several clinical techniques significantly reduce post-procedure discomfort. Occlusal reduction—carefully adjusting your bite—lowers the risk of moderate to severe pain by approximately 40% after instrumentation. This simple adjustment prevents excessive pressure on the treated tooth during healing.
Anxiety management also contributes substantially to pain perception. Options include:
- Nitrous oxide (laughing gas) for mild sedation
- Oral sedatives for moderate anxiety
- Guided breathing techniques
- Comfortable office environment with amenities
Advanced Technologies
Cutting-edge technologies continue to improve pain management in endodontics. Laser endodontic treatments precisely target infected tissue while minimizing trauma to surrounding areas. Cryotherapy—using cold irrigation answers—decreases inflammation and promotes faster healing, resulting in less post-operative discomfort.
Dr. Harris emphasizes that “procedures like pulpotomy and pulpectomy not only treat the infected pulp but actively reduce postoperative pain by removing inflammatory mediators that activate pain receptors.” The combination of thorough root canal debridement with these advanced pain management protocols creates a more comfortable experience for patients throughout their treatment and recovery.
Comparing Endodontic Treatment Options: Which Is Right for You?
Root canal therapy stands as the most common endodontic procedure performed today, serving as the primary option for saving teeth with infected or damaged pulp. During this procedure, dental specialists remove the compromised pulp, thoroughly clean the root canals, and seal them to prevent future infection. Most patients return to normal activities within 24 hours after treatment, and with a success rate exceeding 95%, root canal therapy offers a reliable solution for preserving your natural tooth.
When initial root canal treatment doesn’t resolve the issue or new problems develop, endodontic retreatment becomes necessary. This procedure involves removing the previous filling material, cleaning the canals again, and refilling them to address persistent or new infections. A protective crown typically follows retreatment to strengthen the tooth structure. Dr. Todd B. Harris explains, “Many patients don’t realize that a failed root canal doesn’t automatically mean extraction—retreatment often gives us a second chance to save the natural tooth.”
Endodontic surgery provides answers when conventional treatments aren’t sufficient. Apicoectomy, the most common surgical procedure, removes infected tissue at the root tip and repairs root damage. Surgical intervention may also address hidden canals, fractures, or calcium deposits that conventional treatment can’t reach. Recovery from endodontic surgery typically takes 2-3 days, with success rates ranging from 85-95% depending on case complexity.
The right endodontic treatment for your situation depends on several factors that your dentist will evaluate through clinical examination and X-rays. Initial root canal therapy works best for first-time infections with clear access to all canals. Retreatment becomes the preferred option when previous treatment fails or new infection develops. Surgical approaches like apicoectomy are reserved for cases where conventional treatments aren’t viable or have been unsuccessful.
Sarah M., a recent patient at our practice, shares her experience: “After my initial root canal developed problems years later, I was terrified I’d lose my tooth. Dr. Harris recommended retreatment instead of extraction, and I’m so grateful—the procedure was straightforward, and I’ve had no issues since. Understanding all my options made a huge difference in my decision.”
Specialists in endodontics aim to preserve natural teeth whenever possible by selecting the appropriate procedure based on your exact condition. This personalized approach ensures you receive the most effective treatment while maintaining normal biting force, efficient chewing, and avoiding the need for more extensive tooth replacement options like implants or bridges.
Conclusion
Endodontic treatments like root canals pulpotomies and apicoectomies represent modern dentistry’s commitment to preserving your natural teeth. These procedures have evolved dramatically with advanced technologies making them more comfortable and effective than ever before.
When you experience tooth pain don’t delay seeking treatment. With success rates exceeding 95% for most endodontic procedures you can trust these treatments to eliminate infection relieve pain and save your natural tooth structure.
Remember that preserving your natural teeth offers important advantages for your long-term oral health including maintaining normal bite function and preventing costly replacements. Your endodontist will recommend the most appropriate treatment based on your exact needs ensuring the best possible outcome for your smile.
Frequently Asked Questions
What is endodontic treatment?
Endodontic treatment focuses on the dental pulp and surrounding tissues. It includes procedures like root canals that remove infected pulp to save natural teeth. This treatment becomes necessary when bacteria invade the pulp chamber due to deep decay, repeated dental procedures, cracks, or injuries, causing significant pain and potential abscess formation.
How painful is a root canal procedure?
Despite their intimidating reputation, modern root canal procedures are relatively comfortable. Dentists use effective local anesthetics to numb the area completely before treatment. Most patients experience immediate relief from the severe dental infection pain that brought them in. Post-procedure discomfort is typically mild and manageable with over-the-counter pain medications.
What is the success rate of root canal treatment?
Root canal treatment has a success rate exceeding 95%. Modern techniques and technologies have enhanced both comfort and effectiveness of the procedure. Most treated teeth last a lifetime with proper care, making it a highly reliable option for saving damaged teeth.
How long is the recovery period after a root canal?
Most patients can return to normal activities within 24 hours after root canal treatment. You might experience mild sensitivity for a few days, but severe pain is uncommon and could indicate a problem. Follow your dentist’s post-care instructions, take prescribed medications as directed, and avoid chewing on the treated tooth until restoration is complete.
What is a pulpotomy and who needs it?
A pulpotomy is a less invasive alternative to a full root canal. It involves removing infected pulp only from the crown portion while preserving healthy pulp in the roots. It’s particularly suitable for primary (baby) teeth with extensive decay but no root infection, or for young permanent teeth with immature roots. It can also serve as an emergency measure until a complete root canal can be scheduled.
What is an apicoectomy?
An apicoectomy is an advanced surgical endodontic procedure performed when conventional root canal therapy fails or cannot be redone successfully. It involves surgically removing the tooth root’s tip (apex) to eliminate persistent infections. This procedure gives a second chance to save a tooth before considering extraction, with success rates ranging from 85-95% depending on case complexity.
How is pain managed during and after endodontic procedures?
Pain management during endodontic procedures includes local anesthetics for immediate numbing, medications like NSAIDs and acetaminophen for pain relief, and non-pharmacological methods such as occlusal reduction and anxiety management techniques. Advanced technologies like laser treatments and cryotherapy also help reduce postoperative discomfort, creating a more comfortable experience throughout treatment and recovery.
What happens if a root canal treatment fails?
If initial root canal treatment fails, endodontic retreatment may be necessary. This involves reopening the tooth, removing the previous filling materials, cleaning the canals, and refilling them to address new or persistent infections. If retreatment isn’t possible, an apicoectomy (surgical removal of the root tip) might be recommended. In some cases, extraction may be the only option.
What are the benefits of saving my natural tooth?
Preserving your natural tooth offers numerous benefits, including maintaining normal biting force, efficient chewing, and natural appearance. It prevents shifting of adjacent teeth, preserves jawbone integrity, and eliminates the need for more costly dental implants or bridges. Natural teeth also provide better sensory feedback when chewing and generally require less maintenance than artificial replacements.
How do I know if I need endodontic treatment?
Signs you may need endodontic treatment include severe toothache, prolonged sensitivity to heat or cold, discoloration of the tooth, swelling and tenderness in nearby gums, and persistent or recurring pimple on the gums. Sometimes there are no symptoms, but issues are detected during regular dental checkups. If you experience any of these symptoms, consult your dentist promptly.