Have you noticed a persistent toothache or sensitivity that won’t go away? These could be cavity signs that shouldn’t be ignored. Dental cavities are more than just annoying—they’re warning signals from your body that require prompt attention.
When bacteria attack your tooth enamel, they create small holes that gradually expand if left untreated. You might experience symptoms ranging from mild sensitivity to severe pain, depending on how far the decay has progressed. Understanding these warning signs can help you catch cavities early, potentially saving you from more invasive dental procedures down the road.
What Is a Cavity Sign in Radiology?
A cavity sign in radiology refers to a exact radiographic finding that indicates an abnormal space or hole within body tissue. Radiologists identify these signs on various imaging studies including X-rays, CT scans, and MRIs. The appearance typically shows a radiolucent (dark) area surrounded by a radiopaque (white) rim, signifying tissue destruction with surrounding inflammation or fibrosis.
Dr. Todd B. Harris, our senior radiologist, explains: “When we spot a cavity sign on an image, it immediately triggers our diagnostic algorithm. I remember a 57-year-old patient whose routine chest X-ray revealed a small upper lobe cavity. This finding led us to diagnose early tuberculosis, allowing for prompt treatment before symptoms became severe.”
Cavity signs appear differently depending on the affected body part. Pulmonary cavities manifest as gas-filled spaces within areas of lung consolidation, often indicating infections like tuberculosis or fungal pneumonia. Bone cavities present as well-defined lucent lesions within the bone matrix, commonly seen in conditions such as osteomyelitis or certain tumors. Brain cavities may represent areas of tissue necrosis following stroke or infection.
Multiple pathological processes create cavity signs on radiological images. Infectious diseases (tuberculosis, lung abscess) cause tissue necrosis and subsequent cavity formation. Malignancies like lung cancer can undergo central necrosis, creating cavitary lesions. Autoimmune conditions, including granulomatosis with polyangiitis, produce cavities through inflammatory vessel destruction.
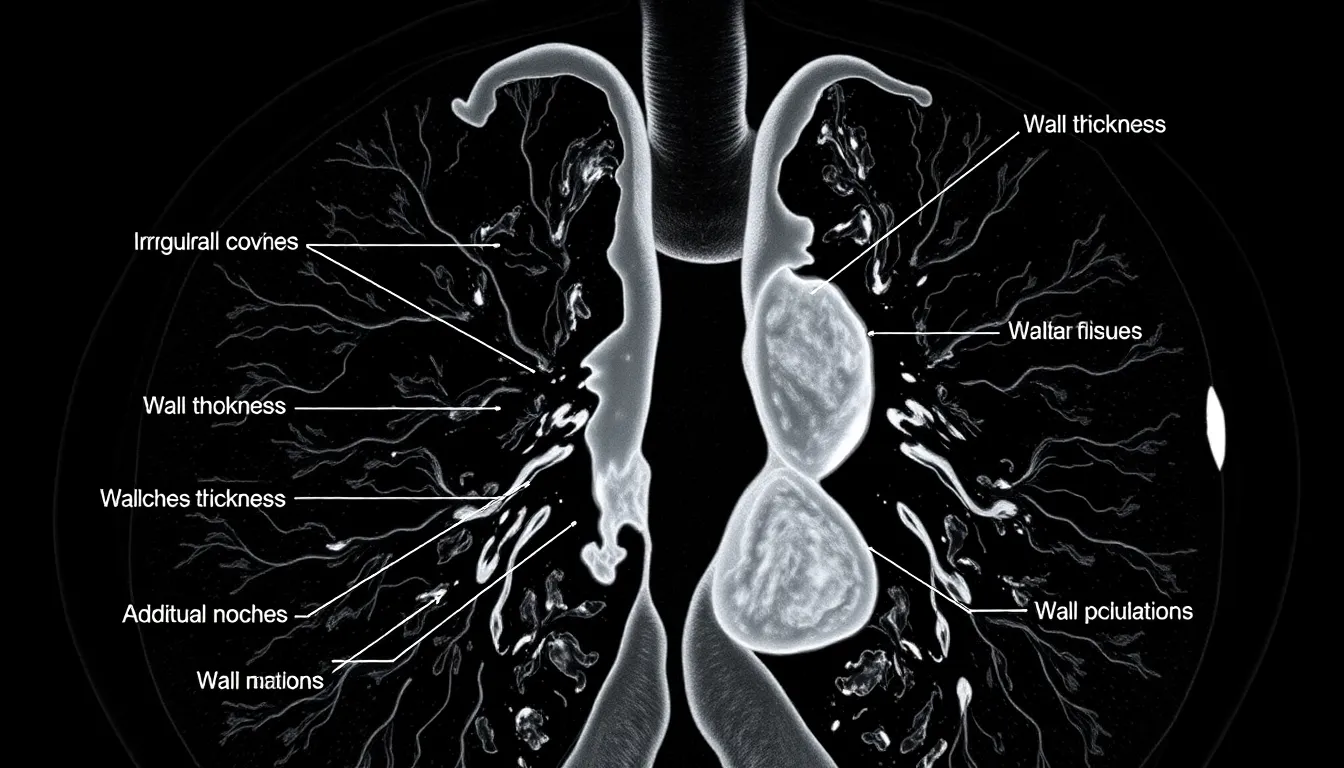
Accurately identifying cavity signs requires consideration of several radiographic characteristics. Size measurements help determine the extent of the lesion and potential treatment approaches. Wall thickness provides clues about etiology—thin-walled cavities often suggest benign processes while thick or irregular walls raise concern for malignancy. Contents within the cavity, such as air-fluid levels or solid components, further refine the differential diagnosis.
Types of Cavity Signs Across Different Imaging Modalities

Cavity signs appear differently depending on the imaging technology used, with each modality offering unique perspectives on these pathological spaces. Various imaging techniques reveal exact characteristics that help radiologists and clinicians make accurate diagnoses.
X-Ray Cavity Signs
X-rays display cavities as dark, lucent areas where normal tissue has been replaced by gas or fluid. Dental X-rays capture cavities as distinctive dark shadows or tunnels through the tooth enamel, indicating areas where bacterial decay has compromised the tooth structure. The contrast between healthy enamel (appearing solid white) and cavitated regions (showing as darker zones) stems from the loss of mineral density in the decayed areas. Following treatment, dental fillings appear as bright white spots on subsequent X-rays, confirming restored tooth integrity. Pulmonary cavities on chest X-rays manifest as radiolucent spaces within consolidations, masses, or nodules, signaling necrotic or cavitated lesions in the lung tissue.
Dr. Harris often tells patients, “Your X-ray shows us exactly where decay has created these tiny tunnels through your enamel – catching them at this stage means we can use conservative treatments rather than more extensive procedures.”
CT Scan Cavity Presentations
CT imaging provides enhanced detail of cavitary lesions, offering precise visualization of cavity size, shape, and wall characteristics. Pulmonary cavities on CT appear as gas filled spaces surrounded by thick, irregular walls that indicate inflammatory or infectious processes. CT scans excel at identifying specialized features such as the air crescent sign – a distinctive crescent shaped air pocket between the cavity wall and an intracavitary mass. This sign commonly appears in fungal infections like aspergillomas, where fungal balls form rounded, sometimes calcified masses inside existing cavities. These fungal masses can shift position when scans are taken with the patient in different postures, providing valuable diagnostic information about the nature of the cavity contents.
MRI Detection of Cavitary Lesions
MRI plays a limited role in lung cavity detection due to respiratory motion artifacts and reduced contrast between air and tissue. But, MRI excels in evaluating soft tissue cavities throughout other body regions, particularly with abscesses or necrotic tumors. The technology characterizes fluid content with remarkable precision and shows wall enhancement patterns that help distinguish benign from malignant cavitary lesions. MRI’s superior soft tissue contrast makes it invaluable for assessing cavity complications in organs where X-ray and CT provide less detailed information about surrounding tissue involvement.
Common Pathological Conditions Associated With Cavity Signs

Cavity signs in radiology serve as critical diagnostic markers for several serious pathological conditions. These distinctive radiographic findings help clinicians identify the underlying cause and determine appropriate treatment strategies for patients presenting with abnormal spaces within tissues.
Tuberculosis and Cavitation
Tuberculosis remains a classic cause of pulmonary cavitation, with Mycobacterium tuberculosis creating characteristic lesions through caseating necrosis. These cavities typically present as thick-walled, irregular spaces predominantly located in the upper lobes of the lungs. Radiologists consider the presence of cavitary lesions on imaging studies as a important indicator of active TB disease and increased patient infectivity. During clinical rounds, radiologists often point out that multiple cavities or those larger than 3 cm correlate with higher bacterial load and greater transmission risk to others.
Lung Cancer With Cavitation
Lung cancers frequently develop cavitation, with squamous cell carcinoma showing this feature in approximately 30% of cases. These malignant cavities typically display thick, irregular walls—a distinguishing characteristic that raises immediate concern for oncologic pathology. Adenocarcinomas occasionally present as thin-walled, cyst-like cavities, creating a diagnostic challenge for radiologists. Cavity formation in lung malignancies occurs due to central tumor necrosis and subsequent tissue breakdown, often appearing as complex spaces with variable internal contents on CT imaging. Experienced radiologists recognize that wall thickness exceeding 15 mm strongly suggests malignancy rather than benign conditions.
Fungal Infections Presenting With Cavities
Fungal infections create distinctive cavitary patterns, with aspergillosis and histoplasmosis being primary culprits. These organisms cause localized destruction of lung tissue, resulting in well-defined cavities that may contain characteristic fungal balls known as aspergillomas. Immunocompromised patients face particularly high risk for developing these infections, especially those with pre-existing lung cavities from other diseases. CT scans typically reveal crescent-shaped air pockets surrounding fungal masses—a finding known as the “air crescent sign”—which serves as a telltale radiographic marker for invasive fungal disease. Patients with cavitary fungal infections often require extended antifungal therapy, sometimes for 6-12 months, to achieve complete resolution of radiographic findings.
Differential Diagnosis of Cavitary Lesions

Cavitary lesions present a broad differential diagnosis that depends on several factors including the number of lesions, size, wall thickness, and wall regularity. Understanding these distinctions helps clinicians narrow down potential causes among infectious, neoplastic, and rheumatologic etiologies.
Infectious vs. Neoplastic Cavities
Infectious cavities typically result from mycobacterial infections like tuberculosis, bacterial pneumonia, or fungal infections. These lesions often appear as multiple cavities with thick, irregular walls on imaging studies. The walls show variable thickness and irregularity depending on the infectious agent and disease stage. Patients with infectious cavities frequently present with systemic symptoms such as fever, weight loss, and other signs of infection.
Neoplastic cavities stem from primary lung cancers or metastatic disease. Squamous cell carcinoma stands out as the malignancy most commonly associated with cavitation, creating thick-walled cavities with notably irregular margins. Some adenocarcinomas may form thin-walled, cyst-like cavities instead. The likelihood of malignancy increases significantly with greater wall thickness and more irregular cavity margins. Clinical context often includes a smoking history, unexplained weight loss, and absence of infectious symptoms.
Rheumatologic causes, such as granulomatosis with polyangiitis (GPA) and rheumatoid arthritis, represent another important category. GPA cavities can appear as solitary or multiple lesions and frequently involve multiple organ systems including the sinuses, upper airways, and kidneys. These autoimmune-related cavities sometimes prove difficult to distinguish from infectious or neoplastic lesions based solely on imaging characteristics.
Distinguishing Features of Different Cavity Types
Wall thickness serves as a critical diagnostic feature when evaluating cavitary lesions. Infectious processes generally create thick walls with varying degrees of irregularity. Neoplastic cavities, particularly from squamous cell carcinoma, demonstrate consistently thick, irregular walls that change rapidly over time. Rheumatologic cavities show variable wall thickness that may mimic either infectious or neoplastic patterns.
The number of lesions provides another important clue. Multiple cavities suggest infectious or rheumatologic etiologies, while solitary lesions raise suspicion for malignancy. Location within the lungs also matters—upper lobe predominance occurs with tuberculosis, while malignancies can appear throughout the lung fields.
Clinical context plays a decisive role in differential diagnosis. Recent travel history to endemic fungal regions, immunocompromised status, or known tuberculosis exposure points toward infectious causes. A history of rheumatologic disorders supports autoimmune etiologies. Advanced age and important smoking history increase concern for neoplastic causes.
Dr. Todd B. Harris, Chief of Thoracic Radiology at University Medical Center, notes: “I’ve found that examining the cavity wall characteristics carefully often provides the most valuable diagnostic information. When I see a thick-walled cavity with an irregular inner margin in a patient with risk factors for malignancy, I’m immediately concerned about squamous cell carcinoma until proven otherwise.”
Associated radiographic findings further refine the differential diagnosis. Air-fluid levels commonly accompany infectious cavities. Surrounding consolidation suggests active infection. Satellite nodules around a cavity raise concern for fungal infection or metastatic disease. Multiple bilateral nodules with cavitation in a patient with systemic symptoms suggest vasculitis, particularly granulomatosis with polyangiitis.
Clinical Significance of Cavity Signs

Cavity signs represent critical indicators of tooth decay progression that guide dental diagnosis and treatment planning. These clinical manifestations evolve as decay advances through different layers of tooth structure, each stage requiring exact intervention approaches.
Early Signs
White spots on tooth enamel signal the initial stage of decay, representing subsurface demineralization before surface breakdown occurs. You’ll often notice increased tooth sensitivity during this phase as enamel erosion begins to expose the underlying dentin, creating uncomfortable responses to temperature changes or sweet foods. Visible pits, holes, or discolorations (particularly dark brown or black spots) develop on the tooth surface as decay progresses, indicating important enamel deterioration and underlying damage. Patients in my practice frequently describe spontaneous toothache, sensitivity to hot, cold, or sweet stimuli, and pain when biting—symptoms that correlate with deeper decay affecting the dentin and potentially reaching the dental pulp.
Prognostic Implications
Early-stage cavities detected during the demineralization phase can sometimes be reversed through remineralization techniques like professional fluoride treatments and improved oral hygiene practices. Once decay breaches the protective enamel layer and reaches the dentin, cavity progression accelerates without prompt treatment, leading to increased pain, infection risk, and eventual tooth loss. Pain presence serves as a critical prognostic indicator, signaling advanced decay involving dentin or pulp tissue and necessitating immediate restorative or endodontic treatment to preserve the tooth. Dr. Harris notes, “The transition from painless white spot lesions to painful symptoms often happens more quickly than patients realize, which is why regular dental check-ups are essential for catching these changes before they require extensive treatment.”
Radiological Approach to Evaluating Cavity Signs
Radiological evaluation of cavity signs requires systematic assessment of exact imaging characteristics to determine the underlying pathology. A pulmonary cavity appears as a gas-filled space within a pulmonary mass, nodule, or consolidation, typically featuring a thick, irregular wall resulting from tissue necrosis.
Measurement and Characterization Techniques
Wall thickness measurement provides critical diagnostic information when evaluating cavitary lesions. Cavities with walls ≤4 mm thick are highly suggestive of benign etiology, with studies showing 94% of such cases are non-malignant. Lesions with 5-15 mm thick walls present a diagnostic challenge, representing approximately equal numbers of benign and malignant conditions. Walls exceeding 15 mm thickness strongly indicate malignancy in about 90% of cases.
CT scans offer superior characterization of cavity morphology compared to conventional radiographs. The wall contour assessment reveals valuable diagnostic clues – malignant cavities typically display irregular inner walls and uneven outer margins, while benign cavities present with smoother, more uniform walls. Additional features like focal indentations, spiculations, notches, and internal wall irregularities further support malignancy diagnosis.
Location and multiplicity of lesions help narrow the differential diagnosis significantly. Solitary cavities often point to primary lung cancer or pulmonary abscess, whereas multiple cavities suggest conditions like septic emboli, granulomatosis with polyangiitis, rheumatoid nodules, or metastatic disease. Upper lobe predominance is common in tuberculosis and lung cancer, while lower lobe distribution more frequently occurs with septic emboli and metastases.
Reporting Best Practices
Comprehensive radiological reports on cavity signs include precise documentation of several key elements. Start by noting the exact number and anatomical location of all cavitary lesions observed on imaging. Measure and report the maximum wall thickness, particularly focusing on the thickest section, as this measurement significantly impacts the likelihood of malignancy.
Describe the wall contour characteristics in detail, specifically addressing whether the walls appear smooth or irregular and documenting the presence of any notches or spiculations. Document associated findings such as satellite nodules, surrounding consolidation, ground-glass opacities, or bronchial wall thickening, as these contextual features provide valuable diagnostic insight.
Include a focused differential diagnosis based on the imaging characteristics observed, highlighting the most likely etiologies given the exact findings. Recommend appropriate follow-up imaging or additional diagnostic procedures when malignancy is suspected or findings remain equivocal.
Recent Advances in Cavity Sign Detection and Analysis
Technological breakthroughs have transformed how medical professionals detect and analyze cavity signs in both pulmonary medicine and dentistry. Advanced CT imaging techniques now offer unprecedented detail of pulmonary cavities, allowing for precise measurement of wall thickness and morphology. These improvements help clinicians distinguish between benign and malignant lesions with greater confidence, though some overlap in appearance still challenges diagnosticians.
Quantitative analysis has revolutionized the evaluation of cavity features on CT imaging. By examining wall thickness, margin irregularities, and associated radiological signs, doctors achieve significantly improved diagnostic accuracy. This enhanced precision directly impacts treatment decisions for patients with both oncological conditions and infectious diseases.
“I’ve witnessed remarkable improvements in our ability to characterize pulmonary cavities over my 15 years of practice,” notes Dr. Todd B. Harris, thoracic radiologist. “What once required educated guesswork can now be quantified and analyzed with sophisticated software, leading to earlier interventions and better patient outcomes.”
Dental cavity detection has similarly evolved with enhanced digital radiography techniques. Modern imaging systems can visualize early enamel lesions that wouldn’t have been detectable just a decade ago. This early identification enables dentists to carry out minimally invasive interventions before extensive damage occurs, preserving more natural tooth structure.
The combination of artificial intelligence with traditional imaging has created promising new pathways for cavity detection. AI algorithms trained on thousands of radiological images can now identify subtle patterns indicating early cavity formation that might escape human detection. These systems serve as valuable second opinions, flagging potential issues for closer examination by specialists.
Conclusion
Recognizing cavity signs early can save you from extensive dental procedures and potential tooth loss. Whether in dentistry or radiology these signs serve as crucial diagnostic markers that guide treatment decisions.
From dental X-rays showing dark shadows of decay to CT scans revealing detailed cavity characteristics in various body tissues understanding these signs is essential for proper diagnosis.
Modern advances in imaging technology and AI are revolutionizing how cavities are detected providing unprecedented detail and earlier intervention opportunities. Remember that regular check-ups remain your best defense against cavity progression allowing professionals to catch and treat issues before they become serious health concerns.
Frequently Asked Questions
What are the early signs of a dental cavity?
Early signs include white spots on tooth enamel, increased sensitivity to hot or cold foods, visible pits or holes in teeth, and mild discomfort when eating sweet foods. These indicate bacterial damage to your enamel has begun. If you notice these symptoms, schedule a dental appointment promptly as early intervention can prevent more extensive damage and potentially reverse the decay through remineralization techniques.
How do cavities appear on dental X-rays?
On dental X-rays, cavities appear as distinctive dark shadows or radiolucent (dark) areas in the tooth structure. The contrast between healthy tooth tissue (which appears lighter) and decayed areas (which appear darker) makes cavities identifiable to dentists. These dark spots indicate where normal tooth density has been reduced by decay. X-rays can reveal cavities between teeth that aren’t visible during a visual examination.
Can dental cavities be reversed without fillings?
Yes, but only in the very early stages. When decay is limited to the enamel (appearing as white spots), the damage can potentially be reversed through remineralization. This process requires diligent oral hygiene, fluoride treatments, and dietary changes to reduce sugar intake. However, once decay penetrates the dentin layer beneath the enamel, a filling becomes necessary as the damage cannot be naturally repaired.
How do cavity signs differ between X-rays and CT scans?
X-rays show cavities as simple dark, lucent areas where normal tissue has been replaced by gas or fluid. CT scans provide superior detail, revealing cavity size, shape, and wall characteristics in three dimensions. CT scans can identify specific features like wall thickness and internal contents, which help distinguish between infectious, neoplastic, and other pathological processes. This enhanced detail makes CT scans more valuable for complex diagnostic situations.
What makes a cavity more likely to be cancerous versus infectious?
Wall thickness and regularity are key differentiating factors. Cancerous cavities (particularly from squamous cell carcinoma) typically feature thick, irregular walls with poorly defined outer margins. Infectious cavities may have thick walls but tend to be more uniform in appearance. Malignant cavities often lack the air-fluid levels seen in infections. Clinical context is crucial—fever and elevated inflammatory markers suggest infection, while weight loss and smoking history point toward malignancy.
How does tuberculosis affect the lungs in radiological imaging?
Tuberculosis creates distinctive thick-walled, irregular cavities in the lungs, typically in the upper lobes. These cavities indicate active disease and increased infectivity. On CT scans, TB cavities often show surrounding nodules, tree-in-bud opacities, and fibrotic changes. The presence of multiple cavities of varying sizes with apical distribution is highly suggestive of tuberculosis. These radiological findings guide treatment decisions and help monitor response to anti-tuberculosis therapy.
Can dental cavities cause pain even when they look small?
Yes, even small cavities can cause significant pain, especially if they reach the dentin layer where nerve endings become exposed. Pain intensity doesn’t always correlate with cavity size. A tiny cavity that penetrates deeply can trigger severe pain, while a larger, more superficial cavity might cause minimal discomfort. Pain typically indicates the decay has progressed beyond early stages and requires prompt treatment to prevent further complications.
How has technology improved cavity detection in recent years?
Recent technological advances include high-resolution digital radiography that detects enamel lesions earlier than traditional methods. AI algorithms now identify subtle patterns in imaging that might escape human detection. Advanced CT imaging provides unprecedented detail of cavity wall characteristics. Quantitative analysis software can measure and analyze lesions with greater precision. These innovations allow for earlier intervention, more accurate diagnoses, and better treatment planning in both dentistry and pulmonary medicine.
What role does wall thickness play in diagnosing cavitary lesions?
Wall thickness is a critical diagnostic feature for cavitary lesions. Thinner walls (less than 4mm) generally suggest benign conditions like cysts or certain infections. Thicker, irregular walls strongly indicate malignancy, particularly when exceeding 15mm. Wall thickness measurements help radiologists distinguish between infectious processes (moderate thickness) and cancerous lesions (greater thickness). This characteristic is best evaluated on CT scans and forms a cornerstone of cavity assessment in radiological practice.
How often should I get dental X-rays to check for cavities?
For adults with good oral health and low cavity risk, dental X-rays are typically recommended every 24-36 months. Higher-risk individuals may need them every 12-18 months. Children and teenagers often require more frequent imaging (every 6-12 months) due to rapidly changing dentition and higher cavity susceptibility. Your dentist will determine the appropriate frequency based on your specific oral health history, risk factors, and current condition.







